Melatonin: A potential therapeutic agent against COVID-19
Melatonin and COVID-19
Abstract
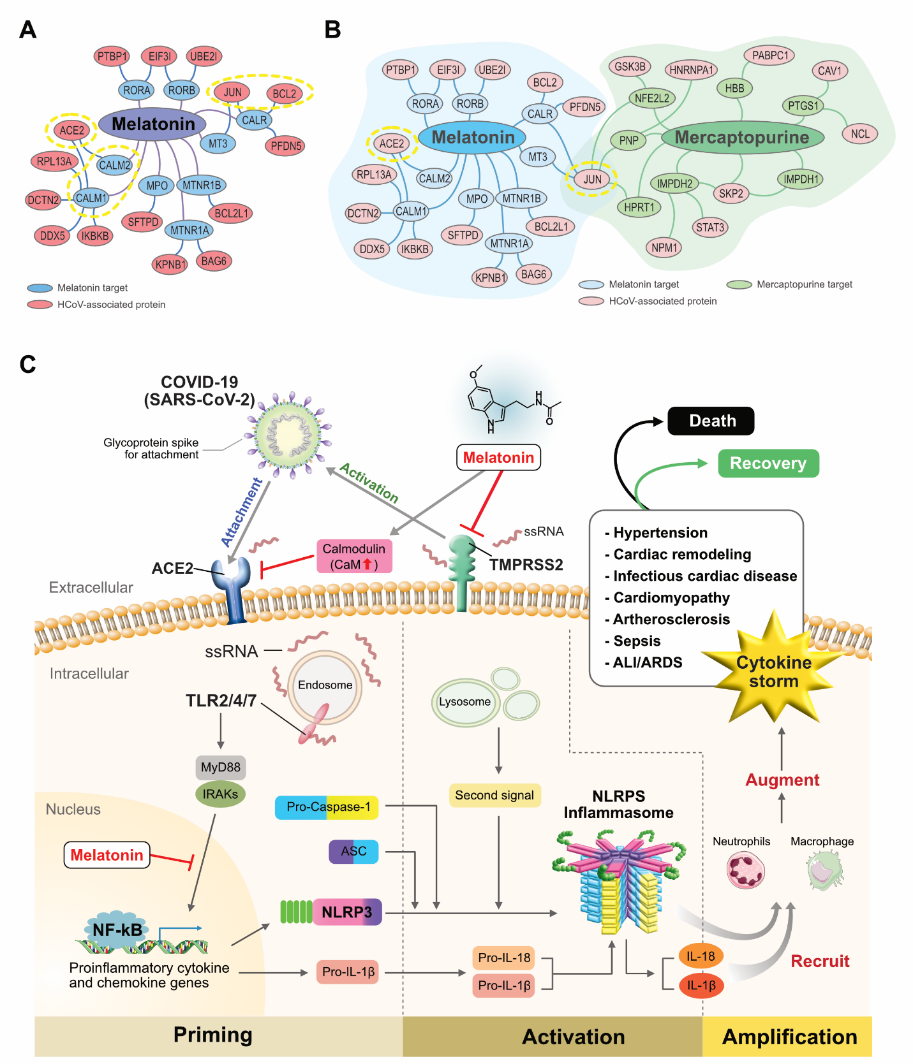
Coronaviruses (CoVs) are RNA viruses that cause infections of the respiratory, gastrointestinal, and central nervous systems, among others. The pathological symptoms of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) include excessive inflammation, elevated oxidative stress, and an exaggerated immune response, ultimately leading to a cytokine storm and subsequent progression to acute lung injury (ALI)/acute respiratory distress syndrome (ARDS) and often, death. Melatonin is a multifunctional and highly significant biomolecule that has anti-inflammatory, anti-oxidative, anti-apoptotic, and neuroprotective actions with no serious undesired side effects, even when administered in high doses. In this review, we present a brief account of the origin of coronaviruses, their characteristic features, infections, transmission, and the causes of coronavirus disease 2019 (COVID-19). We discuss their structure, genome organization, and mechanisms of cellular entry, as well as the pathogenicity of severe acute respiratory syndrome (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2. Furthermore, we provide an account of the typical characteristic features of melatonin, such as its antioxidant, anti-inflammatory, immunomodulatory, and ameliorative effects on various virus-induced infections. Additionally, we identify the rationale for using melatonin as both a prospective adjuvant with vaccine therapy, and as an antiviral immune stimulator. Finally, we provide a perspective on the use of melatonin as a treatment against COVID-19.
References
2. Bande F, Arshad SS, Hair Bejo M, Moeini H, Omar AR. (2015) Progress and challenges toward the development of vaccines against avian infectious bronchitis. J. Immunol. Res. 2015: 424860.
3. Kim Y-I, et al. (2020) Infection and rapid transmission of SARS-CoV-2 in ferrets. Cell Host Microbe 27: 704-709.e702.
4. Zhou P, et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579: 270-273.
5. Zhang R, et al. (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250: 117583.
6. Zhu N, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382: 723-733.
7. Menachery VD, Graham RL, Baric RS. (2017) Jumping species—a mechanism for coronavirus persistence and survival. Curr. Opin. Virol. 23: 1-7.
8. Radogna F, Diederich M, Ghibelli L. (2010) Melatonin: a pleiotropic molecule regulating inflammation. Biochem. Pharmacol. 80: 1844-1852.
9. Hardeland R, et al. (2011) Melatonin--a pleiotropic, orchestrating regulator molecule. Prog. Neurobiol. 93: 350-384.
10. Conti A, et al. (2000) Evidence for melatonin synthesis in mouse and human bone marrow cells. J. Pineal. Res. 28: 193-202.
11. Suofu Y, et al. (2017) Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. 114: E7997-e8006.
12. Tricoire H, Locatelli A, Chemineau P, Malpaux B. (2002) Melatonin enters the cerebrospinal fluid through the pineal recess. Endocrinology 143: 84-90.
13. Lerner AB, Case JD, Takahashi Y, Lee TH, Mori W. (1958) Isolation of melatonin, the pineal gland factor that lightens melanocytes. J. Am. Chem. Soc. 80: 2587-2587.
14. Lerner AB, Case JD, Heinzelman RV. (1959) Structure of melatonin1. J. Am. Chem. Soc. 81: 6084-6085.
15. Reiter RJ. (1993) The melatonin rhythm: both a clock and a calendar. Experientia 49: 654-664.
16. Reiter RJ, Calvo JR, Karbownik M, Qi W, Tan DX. (2000) Melatonin and its relation to the immune system and inflammation. Ann. N. Y. Acad. Sci. 917: 376-386.
17. Reiter RJ, Tan DX, Sainz RM, Mayo JC, Lopez-Burillo S. (2002) Melatonin: reducing the toxicity and increasing the efficacy of drugs. J. Pharm. Pharmacol. 54: 1299-1321.
18. Hardeland R. (2012) Neurobiology, pathophysiology, and treatment of melatonin deficiency and dysfunction. Sci. World J. 2012: 640389.
19. Acuña-Castroviejo D, et al. (2014) Extrapineal melatonin: sources, regulation, and potential functions. Cell Mol. Life Sci. 71: 2997-3025.
20. Hardeland R. (2017) Melatonin and the pathologies of weakened or dysregulated circadian oscillators. J. Pineal. Res. 62: e12377.
21. Lacoste B, et al. (2015) Anatomical and cellular localization of melatonin MT1 and MT2 receptors in the adult rat brain. J. Pineal. Res. 58: 397-417.
22. Ng KY, Leong MK, Liang H, Paxinos G. (2017) Melatonin receptors: distribution in mammalian brain and their respective putative functions. Brain Struct. Funct. 222: 2921-2939.
23. Pinato L, et al. (2017) Day/night expression of MT1 and MT2 receptors in hypothalamic nuclei of the primate Sapajus apella. J. Chem. Neuroanat. 81: 10-17.
24. Nosjean O, et al. (2000) Identification of the melatonin-binding site MT3 as the quinone reductase 2. J. Biol. Chem. 275: 31311-31317.
25. Buryanovskyy L, et al. (2004) Crystal structure of quinone reductase 2 in complex with resveratrol. Biochemistry 43: 11417-11426.
26. Rix U, et al. (2007) Chemical proteomic profiles of the BCR-ABL inhibitors imatinib, nilotinib, and dasatinib reveal novel kinase and nonkinase targets. Blood 110: 4055-4063.
27. Wiesenberg I, Missbach M, Kahlen J-P, Schräder M, Carlberg C. (1995) Transcriptional activation of the nuclear receptor RZRα by the pineal gland hormone melatonin and identification of CGP 52608 as a synthetic ligand. Nucleic Acids Res. 23: 327-333.
28. Salluh JI, et al. (2015) Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ 350: h3129.
29. Mao L, et al. (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 77: 683-690.
30. Zhang Q, Gao F, Zhang S, Sun W, Li Z. (2019) Prophylactic use of exogenous melatonin and melatonin receptor agonists to improve sleep and delirium in the intensive care units: a systematic review and meta-analysis of randomized controlled trials. Sleep Breath. 23: 1059-1070.
31. Zambrelli E, Canevini M, Gambini O, D'Agostino A. (2020) Delirium and sleep disturbances in COVID-19: a possible role for melatonin in hospitalized patients? Sleep Med. 70: 111.
32. Wu G-C, et al. (2020) Melatonin receptor agonist protects against acute lung injury induced by ventilator through up-regulation of IL-10 production. Respir. Res. 21: 65.
33. Maruta H, He H. (2020) PAK1-blockers: potential therapeutics against COVID-19. Med. Drug Discov. 6: 100039-100039.
34. Reiter R, et al. (2019) Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy. Melatonin Res. 2: 105-119.
35. Reiter RJ, et al. (2020) Melatonin inhibits COVID-19-induced cytokine storm by reversing aerobic glycolysis in immune cells: a mechanistic analysis. Med. Drug Discov. 6: 100044.
36. Adiga A, et al. (2020) Evaluating the impact of international airline suspensions on the early global spread of COVID-19. medRxiv.
37. Tesarik J. (2020) After corona: there is life after the pandemic. Reprod. Biomed. Online 40: 760-762.
38. Hui DS, et al. (2020) The continuing epidemic threat of novel coronaviruses to global health-the latest novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 91: 264-266.
39. Ren L-L, et al. (2020) Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin. Med. J. (Engl) 133: 1015-1024.
40. Lu H, Stratton CW, Tang Y-W. (2020) Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 92: 401-402.
41. Cui J, Li F, Shi Z-L. (2019) Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 17: 181-192.
42. van Boheemen S, et al. (2012) Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. MBio 3: e00473-00412.
43. Raj VS, et al. (2013) Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature 495: 251-254.
44. Wang N, et al. (2013) Structure of MERS-CoV spike receptor-binding domain complexed with human receptor DPP4. Cell Res. 23: 986-993.
45. Drucker DJ. (2020) Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr. Rev. 41: bnaa011.
46. Rota PA, et al. (2003) Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science 300: 1394-1399.
47. Yin Y, Wunderink RG. (2018) MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 23: 130-137.
48. Zaki AM, Van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. (2012) Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N. Engl. J. Med. 367: 1814-1820.
49. Park A, Iwasaki A. (2020) Type I and type III Interferons - induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe 27: 870-878.
50. Wu A, et al. (2020) Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe 27: 325-328.
51. Chen L, Zhong L. (2020) Genomics functional analysis and drug screening of SARS-CoV-2. Genes Dis. doi: 10.1016/j.gendis.2020.04.002.
52. Czub M, Weingartl H, Czub S, He R, Cao J. (2005) Evaluation of modified vaccinia virus Ankara based recombinant SARS vaccine in ferrets. Vaccine 23: 2273-2279.
53. Xu X, et al. (2020) Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 63: 457-460.
54. Wan Y, Shang J, Graham R, Baric RS, Li F. (2020) Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 94: e00127-00120.
55. Li H, et al. (2020) SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet 395: 1517-1520.
56. Kim D, et al. (2020) The architecture of SARS-CoV-2 transcriptome. Cell 181: 914-921.e910.
57. Yang D, Leibowitz JL. (2015) The structure and functions of coronavirus genomic 3′ and 5′ ends. Virus Res. 206: 120-133.
58. Konno Y, et al. (2020) SARS-CoV-2 ORF3b is a potent interferon antagonist whose activity is increased by a naturally occurring elongation variant. Cell Rep. 32: 108185.
59. Mousavizadeh L, Ghasemi S. (2020) Genotype and phenotype of COVID-19: their roles in pathogenesis. J. Microbiol. Immunol. Infect. doi: 10.1016/j.jmii.2020.03.022.
60. Wrapp D, et al. (2020) Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 367: 1260-1263.
61. Monteil V, et al. (2020) Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell 181: 905-913.e907.
62. Sola I, Almazan F, Zuniga S, Enjuanes L. (2015) Continuous and discontinuous RNA synthesis in coronaviruses. Annu. Rev. Virol. 2: 265-288.
63. Ziebuhr J (2005) The coronavirus replicase. Coronavirus replication and reverse genetics, (Springer), pp 57-94.
64. Almazán F, et al. (2006) Construction of a severe acute respiratory syndrome coronavirus infectious cDNA clone and a replicon to study coronavirus RNA synthesis. J. Virol. 80: 10900-10906.
65. McIntosh K, Peiris J (2009) Coronaviruses. Clinical Virology, Third Edition, (American Society of Microbiology), pp 1155-1171.
66. Liu C, Xu H, Liu D. (2001) Induction of caspase-dependent apoptosis in cultured cells by the avian coronavirus infectious bronchitis virus. J. Virol. 75: 6402-6409.
67. Mossel EC, et al. (2005) Exogenous ACE2 expression allows refractory cell lines to support severe acute respiratory syndrome coronavirus replication. J. Virol. 79: 3846-3850.
68. Lavi E, Wang Q, Weiss SR, Gonatas NK. (1996) Syncytia formation induced by coronavirus infection is associated with fragmentation and rearrangement of the Golgi apparatus. Virology 221: 325-334.
69. Huang C, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506.
70. Tian X, et al. (2020) Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg. Microbes Infect. 9: 382-385.
71. Fehr AR, Perlman S. (2015) Coronaviruses: an overview of their replication and pathogenesis. Methods Mol. Biol. 1282: 1-23.
72. Gur M, et al. (2020) Exploring conformational transition of 2019 novel coronavirus spike glycoprotein between its closed and open states using molecular dynamics simulations. bioRxiv: 2020.2004.2017.047324.
73. Jaimes JA, Millet JK, Whittaker GR. (2020) Proteolytic cleavage of the SARS-CoV-2 spike protein and the role of the novel S1/S2 site. iScience 23: 101212.
74. Hardeland R, Poeggeler B. (2003) Non-vertebrate melatonin. J. Pineal. Res. 34: 233-241.
75. Pandi‐Perumal SR, et al. (2006) Melatonin: nature's most versatile biological signal? FEBS J. 273: 2813-2838.
76. Remy P, Doder M, Lees A, Turjanski N, Brooks D. (2005) Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 128: 1314-1322.
77. Claustrat B, Brun J, Chazot G. (2005) The basic physiology and pathophysiology of melatonin. Sleep Med. Rev. 9: 11-24.
78. Srinivasan V, Spence DW, Pandi-Perumal SR, Trakht I, Cardinali DP. (2008) Therapeutic actions of melatonin in cancer: possible mechanisms. Integr. Cancer Ther. 7: 189-203.
79. Carlberg C. (2000) Gene regulation by melatonin. Ann. N. Y. Acad. Sci. 917: 387-396.
80. Pariente R, Bejarano I, Espino J, Rodríguez AB, Pariente JA. (2017) Participation of MT3 melatonin receptors in the synergistic effect of melatonin on cytotoxic and apoptotic actions evoked by chemotherapeutics. Cancer Chemother. Pharmacol. 80: 985-998.
81. Maestroni GJ. (2001) The immunotherapeutic potential of melatonin. Expert Opin. Investig. Drugs 10: 467-476.
82. Reiter RJ, et al. (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal. Res. 61: 253-278.
83. Liu L, Labani N, Cecon E, Jockers R. (2019) Melatonin target proteins: too many or not enough? Front. Endocrinol. 10: 791.
84. Pandi-Perumal SR, et al. (2008) The roles of melatonin and light in the pathophysiology and treatment of circadian rhythm sleep disorders. Nat. Clin. Pract. Neurol. 4: 436-447.
85. Cuzzocrea S, et al. (1997) Protective effect of melatonin in carrageenan‐induced models of local inflammation: relationship to its inhibitory effect on nitric oxide production and its peroxynitrite scavenging activity. J. Pineal. Res. 23: 106-116.
86. Hu W, et al. (2017) Utilizing melatonin to combat bacterial infections and septic injury. Br. J. Pharmacol. 174: 754-768.
87. Luo J, et al. (2018) Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. pylori infected mice. Int. Immunopharmacol. 64: 116-122.
88. Ge J, et al. (2019) Melatonin protects intervertebral disc from degeneration by improving cell survival and function via activation of the ERK1/2 signaling pathway. Oxid. Med. Cell. Longev. 2019: 5120275.
89. Chamanara M, et al. (2019) Melatonin ameliorates TNBS-induced colitis in rats through the melatonin receptors: involvement of TLR4/MyD88/NF-κB signalling pathway. Inflammopharmacology 27: 361-371.
90. Xia Y, et al. (2019) Melatonin in macrophage biology: current understanding and future perspectives. J. Pineal. Res. 66: e12547.
91. Hardeland R. (2018) Melatonin and inflammation-story of a double-edged blade. J. Pineal. Res. 65: e12525.
92. Wang QL, et al. (2019) Ginsenoside Rg1 regulates SIRT1 to ameliorate sepsis-induced lung inflammation and injury via inhibiting endoplasmic reticulum stress and inflammation. Mediators Inflamm. 2019: 6453296.
93. Huang S-H, Cao X-J, Liu W, Shi X-Y, Wei W. (2010) Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. J. Pineal. Res. 48: 109-116.
94. Sun CK, et al. (2015) Systemic combined melatonin-mitochondria treatment improves acute respiratory distress syndrome in the rat. J. Pineal. Res. 58: 137-150.
95. Ling Y, et al. (2018) MicroRNA-494 inhibition alleviates acute lung injury through Nrf2 signaling pathway via NQO1 in sepsis-associated acute respiratory distress syndrome. Life Sci. 210: 1-8.
96. Ahmadi Z, Ashrafizadeh M. (2020) Melatonin as a potential modulator of Nrf2. Fundam. Clin. Pharmacol. 34: 11-19.
97. Persengiev SP, Kanchev LN. (1991) Melatonin and adrenal cortex steroid production: in vivo and in vitro studies. Folia Histochem. Cytobiol. 29: 15-18.
98. Lin GJ, et al. (2009) Melatonin prolongs islet graft survival in diabetic NOD mice. J. Pineal. Res. 47: 284-292.
99. Chen S-J, et al. (2016) Melatonin enhances interleukin-10 expression and suppresses chemotaxis to inhibit inflammation in situ and reduce the severity of experimental autoimmune encephalomyelitis. Int. Immunopharmacol. 31: 169-177.
100. Huang S-H, et al. (2019) Melatonin possesses an anti-influenza potential through its immune modulatory effect. J. Funct. Foods. 58: 189-198.
101. Renn TY, et al. (2018) Prophylactic supplement with melatonin successfully suppresses the pathogenesis of periodontitis through normalizing RANKL/OPG ratio and depressing the TLR4/MyD88 signaling pathway. J. Pineal. Res. 64: e12464.
102. Wu X, et al. (2019) Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 axis. Oxid. Med. Cell. Longev. 2019: 4087298.
103. Reiter RJ, Ma Q, Sharma R. (2020) Melatonin in mitochondria: mitigating clear and present dangers. Physiology 35: 86-95.
104. Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ. (2007) One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal. Res. 42: 28-42.
105. Reppert SM, Perlow MJ, Tamarkin L, Klein DC. (1979) A diurnal melatonin rhythm in primate cerebrospinal fluid. Endocrinology 104: 295-301.
106. Guerrero JM, Reiter RJ. (2002) Melatonin-immune system relationships. Curr. Top. Med. Chem. 2: 167-179.
107. Carrillo-Vico A, et al. (2004) Evidence of melatonin synthesis by human lymphocytes and its physiological significance: possible role as intracrine, autocrine, and/or paracrine substance. FASEB J. 18: 537-539.
108. Carrillo-Vico A, Guerrero JM, Lardone PJ, Reiter RJ. (2005) A review of the multiple actions of melatonin on the immune system. Endocrine 27: 189-200.
109. Mauriz JL, Collado PS, Veneroso C, Reiter RJ, González-Gallego J. (2013) A review of the molecular aspects of melatonin's anti-inflammatory actions: recent insights and new perspectives. J. Pineal. Res. 54: 1-14.
110. Poeggeler B, Reiter RJ, Hardeland R, Tan DX, Barlow-Walden LR. (1996) Melatonin and structurally-related, endogenous indoles act as potent electron donors and radical scavengers in vitro. Redox Rep. 2: 179-184.
111. Imai Y, et al. (2008) Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell 133: 235-249.
112. Acuña-Castroviejo D, et al. (2001) Melatonin, mitochondria, and cellular bioenergetics. J. Pineal. Res. 30: 65-74.
113. Jou MJ, et al. (2010) Visualization of melatonin's multiple mitochondrial levels of protection against mitochondrial Ca(2+)-mediated permeability transition and beyond in rat brain astrocytes. J. Pineal. Res. 48: 20-38.
114. Lanari M, Silvestri M, Rossi GA. (2009) Respiratory syncytial virus risk factors in late preterm infants. J. Matern. Fetal Neonatal Med. 22: 102-107.
115. Locksley RM, Killeen N, Lenardo MJ. (2001) The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell 104: 487-501.
116. Xie Q, Nathan C. (1994) The high-output nitric oxide pathway: role and regulation. J. Leukoc. Biol. 56: 576-582.
117. Stark JM, et al. (2005) Immune and functional role of nitric oxide in a mouse model of respiratory syncytial virus infection. J. Infect. Dis. 191: 387-395.
118. Huang SH, Cao XJ, Wei W. (2008) Melatonin decreases TLR3-mediated inflammatory factor expression via inhibition of NF-kappa B activation in respiratory syncytial virus-infected RAW264.7 macrophages. J. Pineal. Res. 45: 93-100.
119. Davis I, Matalon S. (2001) Reactive species in viral pneumonitis: lessons from animal models. News Physiol. Sci. 16: 185-190.
120. Gitto E, et al. (2001) Effects of melatonin treatment in septic newborns. Pediatr. Res. 50: 756-760.
121. Gitto E, et al. (2005) Correlation among cytokines, bronchopulmonary dysplasia and modality of ventilation in preterm newborns: improvement with melatonin treatment. J. Pineal. Res. 39: 287-293.
122. Shao H, et al. (2006) Upregulation of mitochondrial gene expression in PBMC from convalescent SARS patients. J. Clin. Immunol. 26: 546-554.
123. Khomich OA, Kochetkov SN, Bartosch B, Ivanov AV. (2018) Redox biology of respiratory viral infections. Viruses 10: 392.
124. Vijay R, et al. (2015) Critical role of phospholipase A2 group IID in age-related susceptibility to severe acute respiratory syndrome-CoV infection. J. Exp. Med. 212: 1851-1868.
125. Rogers MC, Williams JV. (2019) Reining in the CD8+ T cell: Respiratory virus infection and PD-1-mediated T-cell impairment. PLOS Pathog. 15: e1007387.
126. Yang CY, et al. (2018) New insights into the immune molecular regulation of the pathogenesis of acute respiratory distress syndrome. Int. J. Mol. Sci. 19: 588.
127. Liu J, et al. (2020) Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 55: 102763.
128. Miller SC, Pandi-Perumal SR, Esquifino AI, Cardinali DP, Maestroni GJM. (2006) The role of melatonin in immuno-enhancement: potential application in cancer. Int J Exp Pathol 87: 81-87.
129. Miller SC, Pandi-Perumal SR, Esquifino AI, Cardinali DP, Maestroni GJM. (2006) The role of melatonin in immuno-enhancement: potential application in cancer. Int. J. Exp. Pthol. 87: 81-87.
130. Tate MD, et al. (2016) Reassessing the role of the NLRP3 inflammasome during pathogenic influenza A virus infection via temporal inhibition. Sci. Rep. 6: 27912.
131. Mei SH, et al. (2007) Prevention of LPS-induced acute lung injury in mice by mesenchymal stem cells overexpressing angiopoietin 1. PLOS Med. 4: e269.
132. Shen C, et al. (2019) Molecular mechanism for NLRP6 inflammasome assembly and activation. Proc Natl Acad Sci U S A 116: 2052-2057.
133. Zhang Y, et al. (2016) Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J. Pineal. Res. 60: 405-414.
134. Bryant PA, Trinder J, Curtis N. (2004) Sick and tired: does sleep have a vital role in the immune system? Nat. Rev. Immunol. 4: 457-467.
135. Dhabhar FS. (2009) Enhancing versus suppressive effects of stress on immune function: implications for immunoprotection and immunopathology. Neuroimmunomodulation 16: 300-317.
136. Han Z, Lu W, Huang S. (2007) Synergy effect of melatonin on anti-respiratory syscytical virus activity of ribavirin in vitro. China Pharm. 10:
137. Maestroni GJ, Conti A, Pierpaoli W. (1988) Role of the pineal gland in immunity. III. Melatonin antagonizes the immunosuppressive effect of acute stress via an opiatergic mechanism. Immunology 63: 465-469.
138. Ben-Nathan D, Maestroni G, Lustig S, Conti A. (1995) Protective effects of melatonin in mice infected with encephalitis viruses. Arch. Virol. 140: 223-230.
139. Ibarra-Coronado EG, et al. (2015) Sleep deprivation induces changes in immunity in Trichinella spiralis-infected rats. Int. J. Biol. Sci. 11: 901-912.
140. Habtemariam S, et al. (2017) Melatonin and respiratory diseases: a review. Curr. Top. Med. Chem. 17: 467-488.
141. Safari F, et al. (2020) The interaction of phages and bacteria: the co-evolutionary arms race. Crit. Rev. Biotechnol. 40: 119-137.
142. Prangishvili D, et al. (2017) The enigmatic archaeal virosphere. Nat. Rev. Microbiol. 15: 724-739.
143. Aiewsakun P, Adriaenssens EM, Lavigne R, Kropinski AM, Simmonds P. (2018) Evaluation of the genomic diversity of viruses infecting bacteria, archaea and eukaryotes using a common bioinformatic platform: steps towards a unified taxonomy. J. Gen. Virol. 99: 1331-1343.
144. Horvath P, Barrangou R. (2010) CRISPR/Cas, the immune system of bacteria and archaea. Science 327: 167-170.
145. Bhaya D, Davison M, Barrangou R. (2011) CRISPR-Cas systems in bacteria and archaea: versatile small RNAs for adaptive defense and regulation. Annu. Rev. Genet. 45: 273-297.
146. Hampton HG, Watson BNJ, Fineran PC. (2020) The arms race between bacteria and their phage foes. Nature 577: 327-336.
147. Danilova N. (2006) The evolution of immune mechanisms. J. Exp. Zool. B Mol. Dev. Evol. 306: 496-520.
148. Boehm T, et al. (2018) Evolution of alternative adaptive immune systems in vertebrates. Annu. Rev. Immunol. 36: 19-42.
149. Netea MG, Schlitzer A, Placek K, Joosten LAB, Schultze JL. (2019) Innate and adaptive immune memory: an evolutionary continuum in the host's response to pathogens. Cell Host Microbe 25: 13-26.
150. Tan D-X, Hardeland R. (2020) Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: focus on COVID-19. Melatonin Res. 3: 120-143.
151. Srinivasan S, et al. (2012) Bacterial communities in women with bacterial vaginosis: high resolution phylogenetic analyses reveal relationships of microbiota to clinical criteria. PLOS ONE 7: e37818.
152. Sung PH, et al. (2018) Melatonin attenuated brain death tissue extract-induced cardiac damage by suppressing DAMP signaling. Oncotarget 9: 3531-3548.
153. Luo L, Lucas RM, Liu L, Stow JL. (2019) Signalling, sorting and scaffolding adaptors for Toll-like receptors. J. Cell Sci. 133.
154. Xu X, et al. (2018) Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation. Sci. Rep. 8: 15579.
155. García JA, et al. (2015) Disruption of the NF-κB/NLRP3 connection by melatonin requires retinoid-related orphan receptor-α and blocks the septic response in mice. FASEB J. 29: 3863-3875.
156. Chen Y, Zhou Z, Min W. (2018) Mitochondria, oxidative stress and innate immunity. Front. Physiol. 9: 1487.
157. Tan DX, Manchester LC, Qin L, Reiter RJ. (2016) Melatonin: a mitochondrial targeting molecule involving mitochondrial protection and dynamics. Int. J. Mol. Sci. 17: 2124.
158. Reiter RJ, et al. (2017) Melatonin as a mitochondria-targeted antioxidant: one of evolution's best ideas. Cell Mol. Life Sci. 74: 3863-3881.
159. Tian YM, Zhang GY, Dai YR. (2003) Melatonin rejuvenates degenerated thymus and redresses peripheral immune functions in aged mice. Immunol. Lett. 88: 101-104.
160. Oner H, et al. (2004) Possible effects of melatonin on thymus gland after pinealectomy in rats. Neuro. Endocrinol. Lett. 25: 115-118.
161. Ren W, et al. (2017) Melatonin signaling in T cells: functions and applications. J. Pineal. Res. 62: e12394.
162. Lopez-Gonzalez MA, Lucas M, Sanchez B, Mata F, Delgado F. (1998) Adenoidal and tonsillar lymphocyte subsets in AIDS children. Int. J. Pediatr. Otorhinolaryngol. 45: 215-222.
163. Li J, Cao J, Wang Z, Dong Y, Chen Y. (2015) Melatonin plays a critical role in inducing B lymphocyte proliferation of the bursa of Fabricius in broilers via monochromatic lights. J. Photochem. Photobiol. B 142: 29-34.
164. Ramos A, et al. (2010) Evolution of oxidative/nitrosative stress biomarkers during an open-field vaccination procedure in sheep: effect of melatonin. Vet. Immunol. Immunopathol. 133: 16-24.
165. Hardeland R. (2013) Chronobiology of Melatonin beyond the Feedback to the Suprachiasmatic Nucleus-Consequences to Melatonin Dysfunction. Int. J. Mol. Sci. 14: 5817-5841.
166. Cuzzocrea S, Zingarelli B, Costantino G, Caputi AR. (1998) Protective effect of melatonin in a non‐septic shock model induced by zymosan in the rat. J. Pineal. Res. 25: 24-33.
167. Costantino G, Cuzzocrea S, Mazzon E, Caputi AP. (1998) Protective effects of melatonin in zymosan-activated plasma-induced paw inflammation. Eur. J. Pharmacol. 363: 57-63.
168. Zhao Y, et al. (2019) Melatonin attenuates white matter damage after focal brain ischemia in rats by regulating the TLR4/NF-κB pathway. Brain Res. Bull. 150: 168-178.
169. Gitto E, et al. (2004) Early indicators of chronic lung disease in preterm infants with respiratory distress syndrome and their inhibition by melatonin. J. Pineal. Res. 36: 250-255.
170. Barnham KJ, Masters CL, Bush AI. (2004) Neurodegenerative diseases and oxidative stress. Nat. Rev. Drug Disco. 3: 205-214.
171. Shen C, et al. (2020) Rhein suppresses lung inflammatory injury induced by human respiratory syncytial virus through inhibiting NLRP3 inflammasome activation via NF-κB pathway in mice. Front. Pharmacol. 10: 1600.
172. Akbulut H, Icli F, Büyükcelik A, Akbulut KG, Demirci S. (1999) The role of granulocyte-macrophage-colony stimulating factor, cortisol, and melatonin in the regulation of the circadian rhythms of peripheral blood cells in healthy volunteers and patients with breast cancer. J. Pineal. Res. 26: 1-8.
173. Demas GE, Nelson RJ. (1996) Photoperiod and temperature interact to affect immune parameters in adult male deer mice: (Peromyscus manicuiatus). J. Biol. Rhythms 11: 94-102.
174. Haldar C, Singh R, Guchhait P. (2001) Relationship between the annual rhythms in melatonin and immune system status in the tropical palm squirrel, Funambulus pennanti. Chronobiol. Int. 18: 61-69.
175. Rodriguez AB, Marchena JM, Nogales G, Durán J, Barriga C. (1999) Correlation between the circadian rhythm of melatonin, phagocytosis, and superoxide anion levels in ring dove heterophils. J. Pineal. Res. 26: 35-42.
176. Mackiewicz M, Sollars PJ, Ogilvie MD, Pack AI. (1996) Modulation of IL-1 beta gene expression in the rat CNS during sleep deprivation. Neuroreport 7: 529-533.
177. Lange T, Dimitrov S, Born J. (2010) Effects of sleep and circadian rhythm on the human immune system. Ann. N. Y. Acad. Sci. 1193: 48-59.
178. Touitou Y, Reinberg A, Touitou D. (2017) Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: health impacts and mechanisms of circadian disruption. Life Sci. 173: 94-106.
179. Tan D-X, Reiter RJ. (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2: 44-66.
180. Spiegel K, Sheridan JF, Van Cauter E. (2002) Effect of sleep deprivation on response to immunization. JAMA 288: 1471-1472.
181. Lange T, Perras B, Fehm HL, Born J. (2003) Sleep enhances the human antibody response to hepatitis A vaccination. Psychosom. Med. 65: 831-835.
182. Everson CA. (1993) Sustained sleep deprivation impairs host defense. The American Journal of Physiology 265: R1148-R1154.
183. Teixeira KR, et al. (2019) Night workers have lower levels of antioxidant defenses and higher levels of oxidative stress damage when compared to day workers. Sci. Rep. 9: 1-11.
184. Ramanathan L, Gulyani S, Nienhuis R, Siegel JM. (2002) Sleep deprivation decreases superoxide dismutase activity in rat hippocampus and brainstem. Neuroreport 13: 1387-1390.
185. Hajak G, et al. (1995) Nocturnal plasma melatonin levels in patients suffering from chronic primary insomnia. J. Pineal. Res. 19: 116-122.
186. Cookson BT, Brennan MA. (2001) Pro-inflammatory programmed cell death. Trends Microbiol. 9: 113-114.
187. Panesar NS. (2003) Lymphopenia in SARS. Lancet 361: 1985.
188. Shi CS, Nabar NR, Huang NN, Kehrl JH. (2019) SARS-coronavirus open reading frame-8b triggers intracellular stress pathways and activates NLRP3 inflammasomes. Cell Death Discov. 5: 101.
189. Man SM, Karki R, Kanneganti TD. (2017) Molecular mechanisms and functions of pyroptosis, inflammatory caspases and inflammasomes in infectious diseases. Immunol. Rev. 277: 61-75.
190. Shi J, Gao W, Shao F. (2017) Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem. Sci. 42: 245-254.
191. Zahid A, Li B, Kombe AJK, Jin T, Tao J. (2019) Pharmacological inhibitors of the NLRP3 inflammasome. Front. Immunol. 10: 2538.
192. Wang X, et al. (2019) Melatonin alleviates cigarette smoke-induced endothelial cell pyroptosis through inhibiting ROS/NLRP3 axis. Biochem. Biophys. Res. Commun. 519: 402-408.
193. Arioz BI, et al. (2019) Melatonin attenuates LPS-induced acute depressive-like behaviors and microglial NLRP3 inflammasome activation through the SIRT1/Nrf2 pathway. Front. Immunol. 10: 1511.
194. NaveenKumar SK, Hemshekhar M, Kemparaju K, Girish KS. (2019) Hemin-induced platelet activation and ferroptosis is mediated through ROS-driven proteasomal activity and inflammasome activation: Protection by Melatonin. Biochim. Biophys. Acta Mol. Basis Dis. 1865: 2303-2316.
195. Onk D, et al. (2018) Effect of melatonin on antioxidant capacity, ınflammation and apoptotic cell death in lung tissue of diabetic rats. Acta Cir. Bras. 33: 375-385.
196. Liu Z, et al. (2017) Melatonin alleviates inflammasome-induced pyroptosis through inhibiting NF-κB/GSDMD signal in mice adipose tissue. J. Pineal. Res. 63: e12414.
197. Zarezadeh M, et al. (2020) Melatonin supplementation and pro-inflammatory mediators: a systematic review and meta-analysis of clinical trials. Eur. J. Nutr. 59: 1803-1813.
198. Ellis LC. (1996) Melatonin reduces mortality from Aleutian disease in mink (Mustela vison). J. Pineal. Res. 21: 214-217.
199. Castelruiz Y, Blixenkrone-Møller M, Aasted B. (2005) DNA vaccination with the Aleutian mink disease virus NS1 gene confers partial protection against disease. Vaccine 23: 1225-1231.
200. Laliena A, et al. (2012) Melatonin attenuates inflammation and promotes regeneration in rabbits with fulminant hepatitis of viral origin. J. Pineal. Res. 53: 270-278.
201. Tuñón MJ, et al. (2013) Melatonin treatment reduces endoplasmic reticulum stress and modulates the unfolded protein response in rabbits with lethal fulminant hepatitis of viral origin. J. Pineal. Res. 55: 221-228.
202. Crespo I, et al. (2010) Melatonin prevents the decreased activity of antioxidant enzymes and activates nuclear erythroid 2‐related factor 2 signaling in an animal model of fulminant hepatic failure of viral origin. J. Pineal. Res. 49: 193-200.
203. Tan DX, et al. (2014) Fundamental issues related to the origin of melatonin and melatonin isomers during evolution: relation to their biological functions. Int. J. Mol. Sci. 15: 15858-15890.
204. Anderson G, Maes M, Markus RP, Rodriguez M. (2015) Ebola virus: melatonin as a readily available treatment option. J. Med. Virol. 87: 537-543.
205. Mortezaee K, et al. (2019) Modulation of apoptosis by melatonin for improving cancer treatment efficiency: An updated review. Life Sci. 228: 228-241.
206. Habtemariam S, et al. (2017) Melatonin and respiratory diseases: a review. Curr. Top. Med. Chem. 17: 467-488.
207. Kornblihtt LI, Finocchiaro L, Molinas FC. (1993) Inhibitory effect of melatonin on platelet activation induced by collagen and arachidonic acid. J. Pineal. Res. 14: 184-191.
208. Del Zar MM, et al. (1990) Inhibition of human platelet aggregation and thromboxane-B2 production by melatonin: evidence for a diurnal variation. J. Clin. Endocrinol. Metab. 70: 246-251.
209. Nakao T, et al. (2013) Melatonin ameliorates angiotensin II-induced vascular endothelial damage via its antioxidative properties. J. Pineal. Res. 55: 287-293.
210. Hung MW, et al. (2013) Melatonin ameliorates endothelial dysfunction, vascular inflammation, and systemic hypertension in rats with chronic intermittent hypoxia. J. Pineal. Res. 55: 247-256.
211. Zhang Y, et al. (2018) Melatonin for the treatment of spinal cord injury. Neural. Regen. Res. 13: 1685-1692.
212. Junaid A, et al. (2020) Ebola hemorrhagic shock syndrome-on-a-chip. iScience 23: 100765.
213. Bender BS, Croghan T, Zhang L, Small Jr P. (1992) Transgenic mice lacking class I major histocompatibility complex-restricted T cells have delayed viral clearance and increased mortality after influenza virus challenge. J. Exp. Med. 175: 1143-1145.
214. Anderson G, Reiter RJ. (2020) Melatonin: roles in influenza, Covid-19, and other viral infections. Rev. Med. Virol. 30: e2109.
215. Reiter RJ, et al. (2020) Plasticity of glucose metabolism in activated immune cells: advantages for melatonin inhibition of COVID-19 disease. Melatonin Res. 3: 362-379.
216. Tan DX, Korkmaz A, Reiter RJ, Manchester LC. (2014) Ebola virus disease: potential use of melatonin as a treatment. J. Pineal. Res. 57: 381-384.
217. Holmes EC, Dudas G, Rambaut A, Andersen KG. (2016) The evolution of Ebola virus: Insights from the 2013-2016 epidemic. Nature 538: 193-200.
218. Coltart CE, Lindsey B, Ghinai I, Johnson AM, Heymann DL. (2017) The Ebola outbreak, 2013-2016: old lessons for new epidemics. Philos. Trans. R. Soc. Lond. B Biol. Sci. 372: 20160297.
219. Gałas A. (2014) The determinants of spread of Ebola virus disease - an evidence from the past outbreak experiences. Folia Med. Cracov. 54: 17-25.
220. Mérens A, Bigaillon C, Delaune D. (2018) Ebola virus disease: biological and diagnostic evolution from 2014 to 2017. Med. Mal. Infect. 48: 83-94.
221. Reiter RJ, Ma Q, Sharma R. (2020) Treatment of Ebola and other infectious diseases: melatonin “goes viral”. Melatonin Res. 3: 43-57.
222. Nicastri E, et al. (2019) Ebola virus disease: epidemiology, clinical features, management, and prevention. Infect. Dis. Clin. North Am. 33: 953-976.
223. Murray MJ. (2015) Ebola virus disease: a review of its past and present. Anesth. Analg. 121: 798-809.
224. Tang ST, et al. (2016) Melatonin attenuates aortic endothelial permeability and arteriosclerosis in streptozotocin-induced diabetic rats: possible role of MLCK- and MLCP-dependent MLC phosphorylation. J. Cardiovasc. Pharmacol. Ther. 21: 82-92.
225. Lyon GM, et al. (2014) Clinical care of two patients with Ebola virus disease in the United States. N. Engl. J. Med. 371: 2402-2409.
226. Bah EI, et al. (2015) Clinical presentation of patients with Ebola virus disease in Conakry, Guinea. N. Engl. J. Med. 372: 40-47.
227. Eccles R. (2005) Understanding the symptoms of the common cold and influenza. Lancet Infect. Dis. 5: 718-725.
228. Taubenberger JK, Morens DM. (2008) The pathology of influenza virus infections. Annu. Rev. Pathol. 3: 499-522.
229. Bender BS, Croghan T, Zhang L, Small PA, Jr. (1992) Transgenic mice lacking class I major histocompatibility complex-restricted T cells have delayed viral clearance and increased mortality after influenza virus challenge. J. Exp. Med. 175: 1143-1145.
230. Grunewald ME, Shaban MG, Mackin SR, Fehr AR, Perlman S. (2020) Murine coronavirus infection activates the aryl hydrocarbon receptor in an indoleamine 2,3-dioxygenase-independent manner, contributing to cytokine modulation and proviral TCDD-inducible-PARP expression. J. Virol. 94: e01743-19.
231. Aguiar ACC, et al. (2018) Chloroquine analogs as antimalarial candidates with potent in vitro and in vivo activity. Int. J. Parasitol. Drugs Drug Resist. 8: 459-464.
232. Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. (2003) Effects of chloroquine on viral infections: an old drug against today's diseases. Lancet Infect. Dis. 3: 722-727.
233. Vincent MJ, et al. (2005) Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol. J. 2: 69.
234. Lu H. (2020) Drug treatment options for the 2019-new coronavirus (2019-nCoV). Biosci. Trends 14: 69-71.
235. Agostini ML, et al. (2018) Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. MBio 9: e00221-00218.
236. Holshue ML, et al. (2020) First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 382: 929-936.
237. Wang Z, Chen X, Lu Y, Chen F, Zhang W. (2020) Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined chinese and western medicine treatment. Biosci. Trends 14: 64-68.
238. Lim J, et al. (2020) Case of the index patient who caused tertiary transmission of coronavirus disease 2019 in Korea: The application of lopinavir/ritonavir for the treatment of COVID-19 pneumonia monitored by quantitative RT-PCR. J. Korean Med. Sci. 35: e79.
239. Gordon DE, et al. (2020) A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 583: 459-468.
240. de Wit E, et al. (2020) Prophylactic and therapeutic remdesivir (GS-5734) treatment in the rhesus macaque model of MERS-CoV infection. Proc. Natl. Acad. Sci. 117: 6771-6776.
241. Smith TR, et al. (2020) Immunogenicity of a DNA vaccine candidate for COVID-19. Nat. Commun. 11: 2601.
242. Rajendran K, et al. (2020) Convalescent plasma transfusion for the treatment of COVID‐19: systematic review. J. Med. Virol.: 1-9.
243. Hoffmann M, et al. (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181: 271-280.
244. Guo Y-R, et al. (2020) The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil. Med. Res. 7: 1-10.
245. Paules CI, Marston HD, Fauci AS. (2020) Coronavirus infections-more than just the common cold. JAMA 323: 707-708.
246. Zhou Y, et al. (2020) Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 6: 14.
247. Silvestri GA, et al. (2013) Methods for staging non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: american college of chest physicians evidence-based clinical practice guidelines. Chest 143: e211S-e250S.
248. Tan DX, et al. (2007) Melatonin as a naturally occurring co-substrate of quinone reductase-2, the putative MT3 melatonin membrane receptor: hypothesis and significance. J. Pineal. Res. 43: 317-320.
249. Galano A, Tan DX, Reiter RJ. (2013) On the free radical scavenging activities of melatonin's metabolites, AFMK and AMK. J. Pineal. Res. 54: 245-257.
250. Fung TS, Liu DX. (2017) Activation of the c-Jun NH 2-terminal kinase pathway by coronavirus infectious bronchitis virus promotes apoptosis independently of c-Jun. Cell Death Dis. 8: 1-13.
251. Baghban Rahimi S, et al. (2018) Enhancement of therapeutic DNA vaccine potency by melatonin through inhibiting VEGF expression and induction of antitumor immunity mediated by CD8+ T cells. Arch. Virol. 163: 587-597.
252. Channappanavar R, Perlman S. (2017) Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin. Immunopathol. 39: 529-539.
253. Song P, Li W, Xie J, Hou Y, You C. (2020) Cytokine storm induced by SARS-CoV-2. Clin. Chim. Acta 509: 280-287.
254. Cheung CY, et al. (2005) Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: possible relevance to pathogenesis. J. Virol. 79: 7819-7826.
255. Chu M, et al. (2016) Aberrant expression of novel cytokine IL-38 and regulatory T lymphocytes in childhood asthma. Molecules 21: 933.
256. Law HK, et al. (2005) Chemokine up-regulation in sars-coronavirus–infected, monocyte-derived human dendritic cells. Blood 106: 2366-2374.
257. Tang X, et al. (2020) On the origin and continuing evolution of SARS-CoV-2. Natl. Sci. Rev. 7: 1012–1023.
258. Wong G, et al. (2020) Zoonotic origins of human coronavirus 2019 (HCoV-19 / SARS-CoV-2): why is this work important? Zool. Res. 41: 213-219.
259. Virk RK, et al. (2017) Molecular evidence of transmission of influenza A/H1N1 2009 on a university campus. PLOS ONE 12: e0168596.
260. Petrova VN, Russell CA. (2018) The evolution of seasonal influenza viruses. Nat. Rev. Microbiol. 16: 47-60.
261. Srinivasan V, et al. (2005) Melatonin, immune function and aging. Immun. Ageing 2: 17.
262. Chen Q, Qi WB, Reiter RJ, Wei W, Wang BM. (2009) Exogenously applied melatonin stimulates root growth and raises endogenous indoleacetic acid in roots of etiolated seedlings of Brassica juncea. J. Plant Physiol. 166: 324-328.
263. Carrillo-Vico A, et al. (2006) The modulatory role of melatonin on immune responsiveness. Curr. Opin. Investig. Drugs 7: 423.
264. Wichmann MW, Zellweger R, DeMaso CM, Ayala A, Chaudry IH. (1996) Melatonin administration attenuates depressed immune functions after trauma-hemorrhage. J. Surg. Res. 63: 256-262.
265. Sun YZ, et al. (2015) Assessment of acute lung injury/acute respiratory distress syndrome using B-type brain natriuretic peptide. J. Int. Med. Res. 43: 802-808.
266. Reiter RJ, Abreu-Gonzalez P, Marik PE, Dominguez-Rodriguez A. (2020) Therapeutic algorithm for use of melatonin in patients with COVID-19. Front. Med. 7: 226.
267. Nordlund JJ, Lerner AB. (1977) The effects of oral melatonin on skin color and on the release of pituitary hormones. J. Clin. Endocrinol. Metab. 45: 768-774.
268. Martín Giménez VM, et al. (2020) Lungs as target of COVID-19 infection: protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment. Life Sci. 254: 117808.
269. Yang JK, et al. (2006) Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 23: 623-628.
270. Yang JK, Lin SS, Ji XJ, Guo LM. (2010) Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 47: 193-199.
271. Kulcsar KA, Coleman CM, Beck SE, Frieman MB. (2019) Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection. JCI Insight 4: e131774.
272. Bornstein SR, et al. (2020) Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 8: 546-550.
273. Mehta P, et al. (2020) COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 395: 1033-1034.
274. Simões e Silva AC, Silveira KD, Ferreira AJ, Teixeira MM. (2013) ACE2, angiotensin-(1-7) and Mas receptor axis in inflammation and fibrosis. Br. J. Pharmacol. 169: 477-492.
275. Jaeckel E, Kretschmer K, Apostolou I, von Boehmer H. (2006) Instruction of Treg commitment in peripheral T cells is suited to reverse autoimmunity. Semin. Immunol. 18: 89-92.
276. Ma L, et al. (2020) Effect of SARS-CoV-2 infection upon male gonadal function: A single center-based study. medRxiv: 2020.2003.2021.20037267.
277. Wei L, et al. (2007) Pathology of the thyroid in severe acute respiratory syndrome. Hum. Pathol. 38: 95-102.
278. Srinivasan V, et al. (2013) Metabolic syndrome, its pathophysiology and the role of melatonin. Recent Pat. Endocr. Metab. Immune. Drug Discov. 7: 11-25.
279. Sun H, et al. (2018) Melatonin treatment improves insulin resistance and pigmentation in obese patients with acanthosis nigricans. Int. J. Endocrinol. 2018: 2304746.
280. Owino S, et al. (2018) Nocturnal activation of melatonin receptor type 1 signaling modulates diurnal insulin sensitivity via regulation of PI3K activity. J. Pineal. Res. 64: e12462.
281. Backer JA, Klinkenberg D, Wallinga J. (2020) Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 25: 2000062.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.