Does the melatonin supplementation decrease the severity of the outcomes in COVID-19 patients? A mini review of observational data in the in vivo and in vitro studies
Melatonin and COVID-19
Abstract
The Coronavirus Disease 2019 (COVID-19) is a global pandemic and there is no specific treatment for reducing the severity of this disease up to date. The majority of the treatments remain supportive and empirical. The aim of present study is to assess the relationship between melatonin supplementation and its effect on the severity of the outcomes in covid-19 patients. All published studies up to April 4 of 2021 were searched by using the databases of PubMed, ISI Web of Science, SCOPUS and Google Scholar. Finally, 201 studies have been acquired.
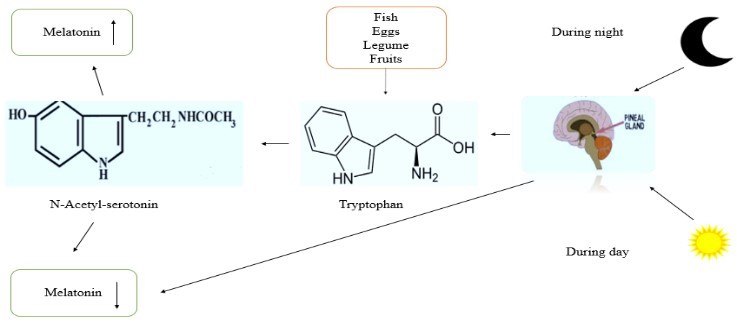
After screening titles, abstracts and justifying the inclusion criteria, eight studies were finally selected in our study. Four studies were observational and case series with total 216,792 participants. Three studies performed on laboratory in the molecular level and one was carried out in mice. The results have suggested that melatonin decreases the severity of the outcomes of COVID-19 patients in their early stage or even in their critical conditions. Furthermore, the melatonin decreases pneumonia and reduces the ground glass lung damage observed in the image findings. Also, it plays an important role as anti-inflammatory, anti-viral and antioxidant activities. Melatonin inhibits the main protease of sares-cov-2 virus and decreases the viral load in molecular level. Regarding the in vivo studies, melatonin is more effective for reducing acute lung injury than other treatments. Although, further clinical studies are required.
References
2. Bai Y, et al. (2020) Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020. 323 (14): 1406-1407.
3. Yang X, et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8 (5): 475-481.
4. Zhou F, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (10229): 1054-1062.
5. Phillips RO, et al. (2020) Rifampicin and clarithromycin (extended release) versus rifampicin and streptomycin for limited Buruli ulcer lesions: a randomised, open-label, non-inferiority phase 3 trial. Lancet 395 (10232): 1259-1267.
6. Menachery VD, et al. (2014) Pathogenic influenza viruses and coronaviruses utilize similar and contrasting approaches to control interferon-stimulated gene responses. mBio 5 (3): e01174-1214.
7. Lau SK, et al. (2013) Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by the novel Middle East respiratory syndrome coronavirus: implications for pathogenesis and treatment. J. Gen. Virol. 94 (Pt 12): 2679-2690.
8. Tang Y, et al. (2020) Cytokine storm in COVID-19: the current evidence and treatment strategies. Front. Immunol. 11: 1708.
9. Phua J, et al. (2020) Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir. Med. 8 (5): 506-517.
10. Zhang R, et al. (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 250:117583.
11. Zhang Y, et al. ( 2016) Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J. Pineal Res. 60 (4): 405-414.
12. Wu G-C, et al. (2020) Melatonin receptor agonist protects against acute lung injury induced by ventilator through up-regulation of IL-10 production. Respir Res. 21 (1): 65.
13. Srinivasan V, Mohamed M, Kato H (2012) Melatonin in bacterial and viral infections with focus on sepsis: a review. Recent Pat. Endocr. Metab. Immune. Drug Discov. 6 (1):30-39.
14. Cardinali DP (2020) High doses of melatonin as a potential therapeutic tool for the neurologic sequels of covid-19 infection. Melatonin Res. 3 (3): 311-317.
15. Murch SJ, Simmons CB (1997) Melatonin in feverfew and other medicinal plants. Lancet 350 (9091): 1598-1599.
16. Oladi E, et al. (2014) Spectrofluorimetric determination of melatonin in kernels of four different Pistacia varieties after ultrasound-assisted solid–liquid extraction. Spectrochim. Acta A Mol. Biomol. Spectrosc. 132: 326-329.
17. Mercolini L, Mandrioli R, Raggi MA (2012), Content of melatonin and other antioxidants in grape‐related foodstuffs: measurement using a MEPS‐HPLC‐F method. J. Pineal Res. 53 (1): p. 21-28.
18. González-Gómez D, et al. (2009) Detection and quantification of melatonin and serotonin in eight sweet cherry cultivars (Prunus avium L.). Eur. Food Res. Technol. 229 (2): 223-229.
19. Stürtz M, et al. (2011) Determination of the melatonin content of different varieties of tomatoes (Lycopersicon esculentum) and strawberries (Fragaria ananassa). Food Chem. 127 (3): 1329-1334.
20. Tan DX, et al. (2014), Melatonin identified in meats and other food stuffs: potentially nutritional impact. J. Pineal Res. 57 (2): 213-218.
21. Karunanithi D, et al. (2014) Quantitative determination of melatonin in milk by LC-MS/MS. J. Food Sci. Technol. 51 (4): 805-812.
22. Milagres MP, et al. (2014) Night milking adds value to cow's milk. J. Sci. Food Agric. 94 (8): 1688-1692.
23. Anisimov VN, et al. (2006) Melatonin as antioxidant, geroprotector and anticarcinogen. Biochim. Biophys. Acta 1757 (5-6): 573-589.
24. Reiter RJ (1996) Antioxidant actions of melatonin. Adv. Pharmacol. 38: 103-117.
25. Rodriguez C, et al. (2004) Regulation of antioxidant enzymes: a significant role for melatonin. J. Pineal Res. 36 (1): 1-9.
26. Korkmaz A, et al. (2009) Melatonin: an established antioxidant worthy of use in clinical trials. Mol. Med. 15 (1): 43-50.
27. Reiter RJ, et al. (2000) Melatonin and its relation to the immune system and inflammation.
Ann. N.Y. Acad. Sci. 917 (1): 376-386.
28. Nabavi SM, et al. (2019) Anti-inflammatory effects of Melatonin: A mechanistic review. Crit. Rev. Food Sci. Nutr. 59 (sup1): S4-S16.
29. Carrillo-Vico A, et al. (2013), Melatonin: buffering the immune system. Int. J. Mol. Sci. 14 (4): 8638-8683.
30. Xia MZ, et al. (2012) Melatonin modulates TLR4‐mediated inflammatory genes through MyD88‐and TRIF‐dependent signaling pathways in lipopolysaccharide‐stimulated RAW264. 7 cells. J. Pineal Res. 53.(4): 325-334.
31. Li Z, et al. (2009) Melatonin protects kidney grafts from ischemia/reperfusion injury through inhibition of NF‐kB and apoptosis after experimental kidney transplantation. J. Pineal Res. 46 (4): 365-372.
32. Hrenak J, et al. (2015) Melatonin and renal protection: novel perspectives from animal experiments and human studies. Curr. Pharm. Des. 21 (7): 936-949.
33. Hardeland R (2019) Aging, melatonin, and the pro-and anti-inflammatory networks.
Int. J. Mol. Sci. 20 (5): 1223.
34. Habtemariam S, et al. (2017) Melatonin and respiratory diseases: a review.
Curr. Top. Med. Chem. 17 (4): 467-488.
35. Hardeland R (2018) Melatonin and inflammation—Story of a double‐edged blade.
J. Pineal Res. 65 (4): e12525.
36. Park JH, et al. (2013) Protective effect of melatonin on TNF‐α‐induced muscle atrophy in L 6 myotubes. J. Pineal Res. 54 (4): 417-425.
37. Sainz R, et al. (2003) Melatonin and cell death: differential actions on apoptosis in normal and cancer cells. Cell. Mol. Life. Sci. 60.(7): 1407-1426.
38. Galano A, Tan DX,. Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: a physicochemical examination. J. Pineal Res. 51 (1): 1-16.
39. Huang S-H, et al. (2019) Melatonin possesses an anti-influenza potential through its immune modulatory effect. J. Funct. Foods. 58: 189-198.
40. Calvo JR, Gonzalez‐Yanes C, Maldonado M (2013) The role of melatonin in the cells of the innate immunity: a review. J. Pineal Res. 55 (2): 103-120.
41. Nordlund JJ, Lerner AB ( 1977) The effects of oral melatonin on skin color and on the release of pituitary hormones. J. Clin. Endocrinol. Metab. 45 (4): 768-774.
42. Li Y, et al. ( 2017) Melatonin for the prevention and treatment of cancer. Oncotarget 8 (24): 39896.
43. Slominski A, et al. (2008) Melatonin in the skin: synthesis, metabolism and functions. Trends Endocrinol. Metab. 19 (1): 17-24.
44. do Carmo Buonfiglio D, et al. (2011) Early-stage retinal melatonin synthesis impairment in streptozotocin-induced diabetic wistar rats. Invest. Ophthalmol. Vis. Sci. 52 ( 10): 7416-7422.
45. Anderson G, Maes M (2015) The gut–brain axis: the role of melatonin in linking psychiatric, inflammatory and neurodegenerative conditions. Adv. Integr. Med. 2 (1): 31-37.
46. Paulose JK, et al. (2016) Human gut bacteria are sensitive to melatonin and express endogenous circadian rhythmicity. PLoS One 11 (1): e0146643.
47. Mukherjee S, Maitra SK (2015) Gut melatonin in vertebrates: chronobiology and physiology. Front. Endocrinol. 6: 112.
48. Carrillo‐Vico A, et al. (2004) Evidence of melatonin synthesis by human lymphocytes and its physiological significance: possible role as intracrine, autocrine, and/or paracrine substance. FASEB J. 18 (3): 537-539.
49. Zhao D, et al. ( 2019) Melatonin Synthesis and Function: Evolutionary History in Animals and Plants. Front. Endocrinol. 10: 249.
50. Markus RP, et al. (2007) The Immune-Pineal Axis: A Shuttle between Endocrine and Paracrine Melatonin Sources. Neuroimmunomodulation 14 (3-4): 126-133.
51. Beriwal N, et al. (2019) Role of immune-pineal axis in neurodegenerative diseases, unraveling novel hybrid dark hormone therapies. Heliyon 5 (1): e01190.
52. Markus RP, et al.(2018) Immune‐pineal axis–acute inflammatory responses coordinate melatonin synthesis by pinealocytes and phagocytes. Br. J. Pharmacol. 175 (16): 3239-3250.
53. Markus RP, Cecon E, Pires-Lapa MA (2013) Immune-pineal axis: nuclear factor κB (NF-kB) mediates the shift in the melatonin source from pinealocytes to immune competent cells. Int. J. Mol. Sci. 14 (6): 10979-10997.
54. Forman K, et al. (2010) Beneficial effects of melatonin on cardiological alterations in a murine model of accelerated aging. J. Pineal Res. 49 (3): 312-320.
55. Wang Y, Chen S, Xu S (2004) Effect of melatonin on the expression of nuclear factor-kappa B and airway inflammation in asthmatic rats. Zhonghua Er Ke Za Zhi 42 (2): 94.
56. Boga JA, et al. ( 2012) Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”? Rev. Med. Virol. 22 (5): 323-338.
57. Anderson G, et al. (2015) Ebola virus: melatonin as a readily available treatment option. J. Med. Virol. 87 (4): 537-543.
58. Bonilla E, et al. (2004) Melatonin and viral infections. J. Pineal Res. 36 (2): 73-79.
59. Turski WA, et al. (2020) AhR and IDO1 in pathogenesis of Covid-19 and the "Systemic AhR Activation Syndrome:" a translational review and therapeutic perspectives. Restor. Neurol. Neurosci. 38 (4): 343-354.
60. Mazzoccoli G, et al. (2020) The Circadian Clock, the Immune System, and Viral Infections: The Intricate Relationship Between Biological Time and Host-Virus Interaction. Pathogens 9: 2.
61. Zhao C, Zhao W (2020) NLRP3 inflammasome—a key player in antiviral responses. Front. Immunol. 11: 211.
62. Wang W, et al. (2018) Zika virus infection induces host inflammatory responses by facilitating NLRP3 inflammasome assembly and interleukin-1β secretion. Nat. Commun. 9 (1): 1-16.
63. Wu H-M, et al. (2020) TLR2-melatonin feedback loop regulates the activation of NLRP3 inflammasome in murine allergic airway inflammation. Front. Immunol. 11: 172.
64. Anderson G, Reiter RJ (2020) Melatonin: roles in influenza, Covid‐19, and other viral infections. Rev. Med. Virol. 30 (3): e2109.
65. Jin CJ, et al. (2016) Sodium butyrate protects mice from the development of the early signs of non-alcoholic fatty liver disease: role of melatonin and lipid peroxidation. Br. J. Nutr. 116 (10): 1682-1693.
66. Wang W, Gao J (2021) Effects of melatonin on protecting against lung injury (Review). Exp. Ther. Med. 21 (3): 228.
67. Pires-Lapa MA, et al. (2018) β-Adrenoceptors trigger melatonin synthesis in phagocytes. Int. J. Mol. Sci. 19: 8.
68. Carvalho‐Sousa CE, et al. (2020) Immune‐pineal axis protects rat lungs exposed to polluted air. J. Pineal Res. 68 (3): e12636.
69. Hardeland R, Tan D.-X (2020) Protection by melatonin in respiratory diseases: valuable information for the treatment of COVID-19. Melatonin Res. 3 (3): 264-275.
70. Zhou Y, et al. (2020) A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLoS Biol. 18 (11): e3000970.
71. Castillo RR, et al. (2020), Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC-19 PRO): a case series. Melatonin Res. 3 (3): 297-310.
72. Feitosa EL, et al. (2020) COVID-19: Rational discovery of the therapeutic potential of Melatonin as a SARS-CoV-2 main Protease Inhibitor. Int. J. Med. Sci. 17 (14): 2133.
73. Jehi L, et al. (2020) Individualizing risk prediction for positive COVID-19 testing: results from 11,672 patients. Chest 158 (4):1364-1375.
74. Al-Zaqri N, et al. (2020) Structural and physico-chemical evaluation of melatonin and its solution-state excited properties, with emphasis on its binding with novel coronavirus proteins. J. Mol. Liq. 318: 114082.
75. Zhang Y, et al. (2016) Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J. Pineal Res. 60 (4): 405-414.
76. Fernandes PA, et al. (2021) Melatonin-Index as a biomarker for predicting the distribution of presymptomatic and asymptomatic SARS-CoV-2 carriers. Melatonin Res. 4 (1): 189-205.
77. Ramlall V, Zucker J, Tatonetti N (2020) Melatonin is significantly associated with survival of intubated COVID-19 patients. medRxiv. 2020.10.15.20213546. doi: 10.1101/2020.10.15.20213546.
78. Tan D-X, Hardeland R (2020) Targeting Host Defense System and Rescuing Compromised Mitochondria to Increase Tolerance against Pathogens by Melatonin May Impact Outcome of Deadly Virus Infection Pertinent to COVID-19. Molecules 25 (19): 4410.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.