Understanding the role of melatonin in cancer metabolism
Melatonin in cancer metabolism
Abstract
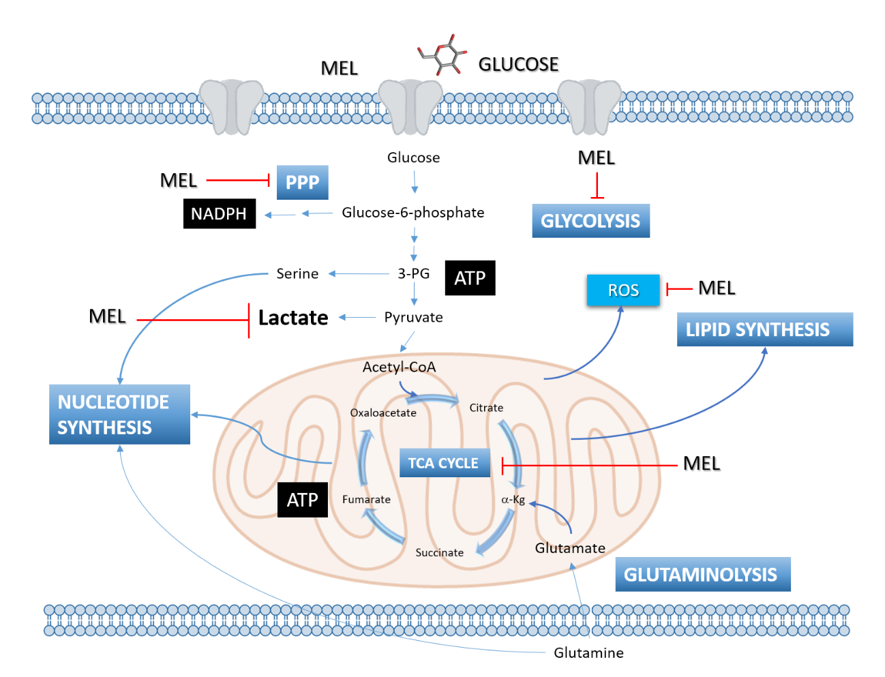
Oncogenes alters metabolic pathways while the resulted metabolites, in turn, modifies the expression and production of oncogenes or tumor suppressors. Metabolic reprogramming has been considered as a consequence of oncogenes’ activity more than a phenotypic change of cancer cells. Currently, three different metabolic alterations for cancer cells, i.e. an increased ability to acquire nutrients, preferred metabolic pathways or differentiation pathways, have been described. Melatonin is a molecule which has been extensively investigated since it was discovered more than 60 years ago. From the aggregation of melanophores to antioxidant chain reactions, melatonin has been proposed to be an important molecule affecting the physiology of mammals but also the biology of unicellular organisms. Thus, the decrease in melatonin synthesis in humans with age has been related to several diseases including neurodegeneration and cancer. For many years, it has been believed that melatonin crosses biological membranes easily to exert its functions. However, this notion has been challenged by recent discovery that majority of melatonin might cross biological membranes through glucose transporters. This initial observation has generated a new important idea about melatonin’s function, that is, the membrane transportation of melatonin and glucose by the same transporter in cancer cells would be a new promising mechanism of this indole by either reprogramming glucose metabolism, impeding nutrients uptake or assigning preferred metabolic pathways in cancer cells. In this review, we will focus the role of melatonin as an antiproliferative agent, and its connection with metabolic changes due to melatonin competition with glucose.
References
factor that lightens melanocytes. J. Am. Chem. Soci. 80: 2587.
2. Hoffman RA, Reiter RJ (1965) Pineal gland: Influence on gonads of male hamsters. Science 148 (3677):1609–1611.
3. Tan DX, et al. (2010) The changing biological roles of melatonin during evolution: From an antioxidant to signals of darkness, sexual selection and fitness. Biol. Rev. 85 (3): 607–623.
4. Reiter RJ (1991) Melatonin: The chemical expression of darkness. Mol. Cell Endocrinol. 79 (1–3):C153-158.
5. Simonneaux V, Ribelayga C (2003) Generation of the melatonin endocrine message in mammals: A review of the complex regulation of melatonin synthesis by norepinephrine, peptides, and other pineal transmitters. Pharmacol. Rev. 55 (2): 325–395.
6. Pévet P (2002) Melatonin. Dialogues Clin Neurosci. 4 (1): 57–72.
7. Pitrosky B, et al. (1991) Effects of different doses and durations of melatonin infusions on plasma melatonin concentrations in pinealectomized Syrian hamsters: Consequences at the level of sexual activity. J. Pineal Res. 11 (3–4): 149–155.
8. Schuhler S, Pitrosky B, Kirsch R, Pévet P (2002) Entrainment of locomotor activity rhythm in pinealectomized adult Syrian hamsters by daily melatonin infusion. Behav. Brain Res. 133 (2): 343–350.
9. Bonmati-Carrion MA, et al. (2014) Protecting the melatonin rhythm through circadian healthy light exposure. Int. J. Mol. Sci. 15 (12): 23448–23500.
10. Reppert SM, et al. (1995) Molecular characterization of a second melatonin receptor expressed in human retina and brain: The Mel(1b) melatonin receptor. Proc. Natl. Acad. Sci. USA 92 (19): 8734–8738.
11. Dubocovich ML, Yun K, Al-Ghoul WM, Benloucif S, Masana MI (1998) Selective MT2 melatonin receptor antagonists block melatonin-mediated phase advances of circadian rhythms. FASEB J. 12 (12): 1211–1220.
12. Nosjean O, et al. (2000) Identification of the melatonin-binding site MT3 as the quinone reductase 2. J. Biol. Chem. 275 (40): 31311–31317.
13. Ebisawa T, Karne S, Lerner MR, Reppert SM (1994) Expression cloning of a high-affinity melatonin receptor from Xenopus dermal melanophores. Proc. Natl. Acad. Sci. USA 91 (13): 6133–6137.
14. Liu J, et al. (2015) MT 1 and MT 2 melatonin receptors: a therapeutic perspective. Annu. Rev. Pharmacol. Toxicol. 56 (1): 361–383.
15. Ferry G, et al. (2010) Old and new inhibitors of quinone reductase 2. Chem. Biol. Interact. 186 (2): 103–109.
16. Levoye A, et al. (2006) The orphan GPR50 receptor specifically inhibits MT1 melatonin receptor function through heterodimerization. EMBO J. 25 (13): 3012–3023.
17. Baba K, et al. (2013) Heteromeric MT1/MT2 melatonin receptors modulate photoreceptor function. Sci. Signal. 6 (296): ra89.
18. Kamal M, et al. (2015) Convergence of melatonin and serotonin (5-HT) signaling at MT2/5-HT2C receptor heteromers. J. Biol. Chem. 290 (18): 11537–11546.
19. Hardeland R, Madrid JA, Tan DX, Reiter RJ (2012) Melatonin, the circadian multioscillator system and health: The need for detailed analyses of peripheral melatonin signaling. J. Pineal Res. 52 (2):139–166.
20. Venegas C, et al. (2012) Extrapineal melatonin: Analysis of its subcellular distribution and daily fluctuations. J. Pineal Res. 52 (2): 217–227.
21. Bubenik GA (2002) Gastrointestinal melatonin: Localization, function, and clinical relevance. Dig. Dis. Sci. 47 (10): 2336–2348.
22. Balzer I, Hardeland R (1991) Photoperiodism and effects of indoleamines in a unicellular alga, Gonyaulax polyedra. Science 253 (5021): 795–797.
23. Tan DX, Chen L-D, Poeggeler B, Manchester LC, Reiter RJ (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr. J. 1:57–60.
24. Reiter RJ, et al. (2003) Melatonin: detoxification of oxygen and nitrogen-based toxic reactants. Adv. Exp. Med. Biol. 527: 539–348.
25. Galano A, Tan DX, Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: A physicochemical examination. J. Pineal Res. 51 (1):1–16.
26. Manchester LC, et al. (2015) Melatonin: An ancient molecule that makes oxygen metabolically tolerable. J. Pineal Res. 59 (4):403–419.
27. Sainz RM, et al. (2000) Changes in lipid peroxidation during pregnancy and after delivery in rats: Effect of pinealectomy. J. Reprod. Fertil. 119 (1): 143-149.
28. García JJ, et al. (2014) Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: A review. J. Pineal Res. 56 (3): 225–237.
29. Mayo JC, Tan D-X, Sainz RM, Lopez-Burillo S, Reiter RJ (2003) Oxidative damage to catalase induced by peroxyl radicals: functional protection by melatonin and other antioxidants. Free Radic. Res. 37 (5): 543–553.
30. Tan DX, et al. (1993) The pineal hormone melatonin inhibits DNA-adduct formation induced by the chemical carcinogen safrole in vivo. Cancer Lett. 70 (1–2): 65–71.
31. Tan DX, et al. (1994) Both physiological and pharmacological levels of melatonin reduce DNA adduct formation induced by the carcinogen safrole. Carcinogenesis 15 (2): 215–218.
32. Pappolla MA, et al. (1999) Alzheimer β protein mediated oxidative damage of mitochondrial DNA: Prevention by melatonin. J. Pineal Res. 27 (4): 226–229.
33. Tan DX, Manchester LC, Terron MP, Flores LJ, Reiter RJ (2007) One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 42 (1): 28–42.
34. Abe M, Reiter RJ, Orhii PB, Hara M, Poeggeler B (1994) Inhibitory effect of melatonin on cataract formation in newborn rats: Evidence for an antioxidative role for melatonin. J. Pineal Res. 17 (2): 94–100.
35. Mayo JC, et al. (2002) Melatonin regulation of antioxidant enzyme gene expression. Cell Mol. Life Sci. 59 (10): 1706–1713.
36. Chen Y, et al. (2015) Melatonin protects hepatocytes against bile acid-induced mitochondrial oxidative stress via the AMPK-SIRT3-SOD2 pathway. Free Radic. Res. 49 (10): 1275–1284.
37. Choi S Il, Dadakhujaev S, Ryu H, Im Kim T, Kim EK (2011) Melatonin protects against oxidative stress in granular corneal dystrophy type 2 corneal fibroblasts by mechanisms that involve membrane melatonin receptors. J. Pineal Res. 51 (1):94–103.
38. Wang J, et al. (2015) Clock-controlled StAR’s expression and corticosterone production contribute to the endotoxemia immune response. Chronobiol. Int. 32 (3):358-367. doi: 10.3109/07420528.
39. Hevia D, et al. (2008) Melatonin uptake in prostate cancer cells: Intracellular transport versus simple passive diffusion. J. Pineal Res. 45 (3):247–257.
40. Hevia D, Mayo JC, Quiros I, Gomez-Cordoves C, Sainz RM (2010) Monitoring intracellular melatonin levels in human prostate normal and cancer cells by HPLC. Anal. Bioanal. Chem. 397 (3):1235–1244.
41. Nguyen J, Wright KP (2010) Influence of weeks of circadian misalignment on leptin levels. Nat. Sci. Sleep 2: 9–18.
42. Nduhirabandi F, Du Toit EF, Blackhurst D, Marais D, Lochner A (2011) Chronic melatonin consumption prevents obesity-related metabolic abnormalities and protects the heart against myocardial ischemia and reperfusion injury in a prediabetic model of diet-induced obesity. J. Pineal Res. 50 (2):171–182.
43. Agil A, et al. (2012) Melatonin improves glucose homeostasis in young Zucker diabetic fatty rats. J. Pineal Res. 52 (2): 203–210.
44. Karamitri A, Jockers R (2019) Melatonin in type 2 diabetes mellitus and obesity. Nat. Rev. Endocrinol. 15 (2):105-125. doi: 10.1038/s41574-018-0130-1.
45. Goyal A, et al. (2014) Melatonin supplementation to treat the metabolic syndrome: A randomized controlled trial. Diabetol. Metab. Syndr. 6 (1):124.
46. Amstrup AK, et al. (2016) Reduced fat mass and increased lean mass in response to 1 year of melatonin treatment in postmenopausal women: A randomized placebo-controlled trial. Clin. Endocrinol. (Oxf) 84 (3):342–347.
47. Buonfiglio D, et al. (2019) Removing melatonin receptor type 1 signaling leads to selective leptin resistance in the arcuate nucleus. J. Pineal Res. e: 12580.
48. Nogueira TC, et al. (2011) Absence of melatonin induces night-time hepatic insulin resistance and increased gluconeogenesis due to stimulation of nocturnal unfolded protein response. Endocrinology 152 (4): 1253–1263.
49. Sartori C, et al. (2009) Melatonin improves glucose homeostasis and endothelial vascular function in high-fat diet-fed insulin-resistant mice. Endocrinology 150 (12): 5311–5317.
50. Kadhim HM, et al. (2006) Effects of melatonin and zinc on lipid profile and renal function in type 2 diabetic patients poorly controlled with metformin. J. Pineal Res. 41 (2):189–193.
51. Zisapel N, et al. (2011) Efficacy and safety of prolonged-release melatonin in insomnia patients with diabetes: a randomized, double-blind, crossover study. Diabetes Metab. Syndr. Obes. Targets Ther. 4: 307.
52. Contreras-Alcantara S, Baba K, Tosini G (2010) Removal of melatonin receptor type 1 induces insulin resistance in the mouse. Obesity (Silver Spring) 18 (9): 1861–1863.
53. Lyssenko V, et al. (2009) Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat. Genet. 41 (1):82–88.
54. Bartsch C, et al. (1997) Nocturnal urinary 6-sulphatoxymelatonin excretion is decreased in primary breast cancer patients compared to age-matched controls and shows negative correlation with tumor-size. J. Pineal Res. 23 (2): 53–58.
55. Grin W, Grünberger W (1998) A significant correlation between melatonin deficiency and endometrial cancer. Gynecol. Obstet. Invest. 45 (1): 62–65.
56. Viswanathan AN, Schernhammer ES (2009) Circulating melatonin and the risk of breast and endometrial cancer in women. Cancer Lett. 281 (1): 1–7.
57. Bartsch C, et al. (2000) Serial transplants of DMBA-induced mammary tumors in Fischer rats as model system for human breast cancer: V. Myoepithelial-mesenchymal conversion during passaging as possible cause for modulation of pineal-tumor interaction. Exp. Toxicol. Pathol. 52 (2): 93–101.
58. Karasek M, Kowalski AJ, Suzin J, Zylinska K, Swietoslawski J (2005) Serum melatonin circadian profiles in women suffering from cervical cancer. J. Pineal Res. 39 (1): 73–76.
59. Schernhammer ES, Hankinson SE (2005) Urinary melatonin levels and breast cancer risk. J. Natl. Cancer Inst. 97 (14): 1084–1087.
60. Reiter RJ, et al. (2007) Light at night, chronodisruption, melatonin suppression, and cancer risk: a review. Crit. Rev. TM Oncog. 13 (4): 303–328.
61. Blask DE, Sauer L, Dauchy RT (2002) Melatonin as a chronobiotic/anticancer agent: cellular, biochemical, and molecular mechanisms of action and their implications for circadian-based cancer therapy. Curr. Top. Med. Chem. 2 (2):113–132.
62. Mediavilla D, Sanchez-Barcelo MJ E, Tan DX, Manchester L, Reiter RJ (2011) Basic mechanisms involved in the anti-cancer effects of melatonin. Curr. Med. Chem. 17 (36): 4462–4481.
63. Tan DX, et al. (2003) Melatonin: a hormone, a tissue factor, an autocoid, a paracoid, and an antioxidant vitamin. J. Pineal Res. 34 (1):75–78.
64. Tan DX, et al. (1999) High physiological levels of melatonin in the bile of mammals. Life Sci. 65 (23): 2523–2529.
65. Skinner DC, Malpaux B (1999) High melatonin concentrations in third ventricular cerebrospinal fluid are not due to Galen vein blood recirculating through the choroid plexus. Endocrinology 140 (10): 4399–4405.
66. Tan DX, Manchester LC, Reiter RJ (2016) CSF generation by pineal gland results in a robust melatonin circadian rhythm in the third ventricle as an unique light/dark signal. Med. Hypotheses 86: 3–9.
67. Acuña-Castroviejo D, et al. (2014) Extrapineal melatonin: Sources, regulation, and potential functions. Cell Mol. Life Sci. 71 (16):2997–3025.
68. Danielczyk K, Dziegiel P (2009) The expression of MT1 melatonin receptor and Ki-67 antigen in melanoma malignum. Anticancer Res. 29 (10): 3887–3895.
69. Jablonska K, et al. (2013) Expression of melatonin receptor MT1 in cells of human invasive ductal breast carcinoma. J. Pineal Res. 54 (3): 334–345.
70. Ying SW, Niles LP, Crocker C (1993) Human malignant melanoma cells express high-affinity receptors for melatonin: antiproliferative effects of melatonin and 6-chloromelatonin. Eur. J. Pharmacol. 246 (2): 89–96.
71. Blask DE, et al. (1999) Melatonin inhibition of cancer growth in vivo involves suppression of tumor fatty acid metabolism via melatonin receptor-mediated signal transduction events. Cancer Res. 59 (18): 4693–4701.
72. Blask DE, Hill SM (1986) Effects of melatonin on cancer: studies on MCF-7 human breast cancer cells in culture. J. Neural. Transm. Suppl. 21: 433–449.
73. Tam CW, et al. (2008) Melatonin as a negative mitogenic hormonal regulator of human prostate epithelial cell growth: Potential mechanisms and clinical significance. J. Pineal Res. 45 (4): 403–412.
74. Xi SC, Siu SWF, Fong SW, Shiu SYW (2001) Inhibition of androgen-sensitive LNCaP prostate cancer growth in vivo by melatonin: Association of antiproliferative action of the pineal hormone with MT1 receptor protein expression. Prostate 46 (1): 52–61.
75. Leja-Szpak A, et al. (2015) Kynuramines induce overexpression of heat shock proteins in pancreatic cancer cells via 5-hydroxytryptamine and MT1/MT2 receptors. J. Physiol. Pharmacol. 66 (5): 711–718.
76. Pan Y, Niles LP (2015) Epigenetic mechanisms of melatonin action in human SH-SY5Y neuroblastoma cells. Mol. Cell Endocrinol. 402: 57–63.
77. Yuan L, Collins AR, Dai J, Dubocovich ML, Hill SM (2002) MT1 melatonin receptor overexpression enhances the growth suppressive effect of melatonin in human breast cancer cells. Mol. Cell Endocrinol. 192 (1–2): 147–156.
78. Mao L, et al. (2010) Inhibition of breast cancer cell invasion by melatonin is mediated through regulation of the p38 mitogen-activated protein kinase signaling pathway. Breast Cancer Res. 12 (6): R107.
79. Treeck O, Haldar C, Ortmann O (2006) Antiestrogens modulate MT1 melatonin receptor expression in breast and ovarian cancer cell lines. Oncol. Rep. 15 (1): 231–235.
80. Zonta YR, et al. (2017) Melatonin reduces angiogenesis in serous papillary ovarian carcinoma of ethanol-preferring rats. Int. J. Mol. Sci. 18 (4): 763.
81. Chuffa LG de A, Reiter RJ, Lupi LA (2017) Melatonin as a promising agent to treat ovarian cancer: Molecular mechanisms. Carcinogenesis 38 (10):945–952.
82. Akbarzadeh M, et al. (2017) The potential therapeutic effect of melatonin on human ovarian cancer by inhibition of invasion and migration of cancer stem cells. Sci, Rep, 7 (1):17062.
83. Santoro R, Marani M, Blandino G, Muti P, Strano S (2012) Melatonin triggers p53Ser phosphorylation and prevents DNA damage accumulation. Oncogene 31 (24): 2931–2942.
84. Santoro R, et al. (2013) Blockage of melatonin receptors impairs p53-mediated prevention of DNA damage accumulation. Carcinogenesis 34 (5):1051–1061.
85. Marengo B, et al. (2016) Redox homeostasis and cellular antioxidant systems: Crucial players in cancer growth and therapy. Oxid. Med. Cell Longev. 2016: 1–16.
86. Holmström KM, Finkel T (2014) Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat. Rev. Mol. Cell Biol. 15 (6): 411–421.
87. Vijayalaxmi, Reiter RJ, Herman TS, Meltz ML (1998) Melatonin reduces gamma radiation-induced primary DNA damage in human blood lymphocytes. Mutat. Res. Fundam. Mol. Mech. Mutagen 397 (2):203–208.
88. Cadenas S, Barja G (1999) Resveratrol, melatonin, vitamin E, and PBN protect against renal oxidative DNA damage induced by the kidney carcinogen KBrO3. Free Radic. Biol. Med. 26 (11–12): 1531–1537.
89. Sainz RM, et al. (2003) Antioxidant activity of melatonin in Chinese hamster ovarian cells: changes in cellular proliferation and differentiation. Biochem. Biophys. Res. Commun. 302 (3): 625–634.
90. Sainz RM, et al. (2005) Melatonin reduces prostate cancer cell growth leading to neuroendocrine differentiation via a receptor and PKA independent mechanism. Prostate 63 (1): 29–43.
91. Hevia D, et al. (2015) Melatonin uptake through glucose transporters: A new target for melatonin inhibition of cancer. J. Pineal Res. 58 (2): 234–250.
92. Wang J, et al. (2012) Melatonin suppresses migration and invasion via inhibition of oxidative stress pathway in glioma cells. J. Pineal Res. 53 (2): 180–187.
93. Ordoñez R, et al. (2014) Inhibition of matrix metalloproteinase-9 and nuclear factor kappa B contribute to melatonin prevention of motility and invasiveness in HepG2 liver cancer cells. J. Pineal Res. 56 (1): 20–30.
94. Yeh CM, et al. (2016) Melatonin inhibits TPA-induced oral cancer cell migration by suppressing matrix metalloproteinase-9 activation through the histone acetylation. Oncotarget 7 (16): 21952–21967.
95. Rudra DS, Pal U, Maiti NC, Reiter RJ, Swarnakar S (2013) Melatonin inhibits matrix metalloproteinase-9 activity by binding to its active site. J. Pineal Res. 54 (4): 398–405.
96. Trivedi PP, Jena GB, Tikoo KB, Kumar V (2016) Melatonin modulated autophagy and Nrf2 signaling pathways in mice with colitis-associated colon carcinogenesis. Mol. Carcinog. 55 (3):255–267.
97. Reiter RJ, Tan D-X, Sainz RM, Mayo JC, Lopez-Burillo S (2002) Melatonin: reducing the toxicity and increasing the efficacy of drugs. J. Pharm. Pharmacol. 54 (10): 1299–321.
98. Kelland L (2007) The resurgence of platinum-based cancer chemotherapy. Nat. Rev. Cancer 7 (8): 573–584.
99. Jang H, et al. (2016) Melatonin prevents cisplatin-induced primordial follicle loss via suppression of PTEN/AKT/FOXO3a pathway activation in the mouse ovary. J. Pineal Res. 60 (3): 336–347.
100. Rapozzi V, et al. (1998) Melatonin decreases bone marrow and lymphatic toxicity of adriamycin in mice bearing TLX5 lymphoma. Life Sci. 63 (19): 1701–1713.
101. Kim C, et al. (2005) Modulation by melatonin of the cardiotoxic and antitumor activities of adriamycin. J. Cardiovasc. Pharmacol. 46 (2): 200–210.
102. Öz E, Erbaş D, Sürücü HS, Düzgün E (2006) Prevention of doxorubicin-induced cardiotoxicity by melatonin. Mol. Cell Biochem. 282 (1–2): 31–37.
103. Govender J, Loos B, Marais E, Engelbrecht AM (2014) Mitochondrial catastrophe during doxorubicin-induced cardiotoxicity: A review of the protective role of melatonin. J. Pineal Res. 57 (4): 367–380.
104. Pariente R, Pariente JA, Rodríguez AB, Espino J (2016) Melatonin sensitizes human cervical cancer HeLa cells to cisplatin-induced cytotoxicity and apoptosis: Effects on oxidative stress and DNA fragmentation. J. Pineal Res. 60 (1): 55–64.
105. Uguz AC, et al. (2012) Melatonin potentiates chemotherapy-induced cytotoxicity and apoptosis in rat pancreatic tumor cells. J. Pineal Res. 53 (1): 91–98.
106. Hevia D, Mayo JC, Tan DX, Rodriguez-Garcia A, Sainz RM (2014) Melatonin enhances photo-oxidation of 2',7'-dichlorodihydrofluorescein by an antioxidant reaction that renders N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK). PLoS One 9 (10): e109257.
107. Rasola A, Bernardi P (2014) The mitochondrial permeability transition pore and its adaptive responses in tumor cells. Cell Calcium. 56 (6):437–445.
108. Li W, et al. (2015) Melatonin induces cell apoptosis in AGS cells through the activation of JNK and P38 MAPK and the suppression of nuclear Factor-Kappa B: A novel therapeutic implication for gastric cancer. Cell Physiol. Biochem. 37 (6): 2323–2338.
109. Sainz RM, et al. (2008) Critical role of glutathione in melatonin enhancement of tumor necrosis factor and ionizing radiation-induced apoptosis in prostate cancer cells in vitro. J. Pineal Res. 45 (3): 258–270.
110. Shen HM, Tergaonkar V (2009) NFκB signaling in carcinogenesis and as a potential molecular target for cancer therapy. Apoptosis 14 (4): 348–363.
111. Ben-Neriah Y, Karin M (2011) Inflammation meets cancer, with NF-κB as the matchmaker. Nat. Immunol. 12 (8):715–723.
112. Surcel CI, et al. (2015) Prognostic effect of neuroendocrine differentiation in prostate cancer: A critical review. Urol. Oncol. Semin. Orig. Investig. 33 (6): 265.e1-265.e7.
113. Rodriguez-Garcia A, et al. (2013) Phenotypic changes caused by melatonin increased sensitivity of prostate cancer cells to cytokine-induced apoptosis. J. Pineal Res. 54 (1): 33–45.
114. Hardeland R (2018) Melatonin and retinoid orphan receptors: Demand for new interpretations after their exclusion as nuclear melatonin receptors. Melatonin Res. 1 (1): 78–93.
115. Danforth DN, Tamarkin L, Lippman ME (1983) Melatonin increases oestrogen receptor binding activity of human breast cancer cells. Nature 305 (5932): 323–325.
116. Hill SM, Blask DE (1988) Effects of the pineal hormone melatonin on the proliferation and morphological characteristics of human breast cancer cells (MCF-7) in culture. Cancer Res. 48 (21):6121–6126.
117. Wilson ST, Blask DE, Lemus-Wilson AM (1992) Melatonin augments the sensitivity of MCF-7 human breast cancer cells to tamoxifen in vitro. J. Clin. Endocrinol. Metab. 75 (2): 669–670.
118. Cos S1, Fernández R, Güézmes A, Sánchez-Barceló EJ (1998) Influence of melatonin on invasive and metastatic properties of MCF-7 human breast cancer cells. Cancer Res. 58 (19):4383–4390.
119. Cos S, Mediavilla MD, Fernández R, González-Lamuño D, Sánchez-Barceló EJ (2002) Does melatonin induce apoptosis in MCF-7 human breast cancer cells in vitro? J. Pineal Res. 32 (2): 90–96.
120. Alvarez-García V, González A, Alonso-González C, Martínez-Campa C, Cos S (2013) Regulation of vascular endothelial growth factor by melatonin in human breast cancer cells. J. Pineal Res. 54 (4): 373–380.
121. Cos S, Martínez-Campa C, Mediavilla MD, Sánchez-Barceló EJ (2005) Melatonin modulates aromatase activity in MCF-7 human breast cancer cells. J. Pineal Res. 38 (2): 136–142.
122. Proietti S, et al. (2014) Melatonin down-regulates MDM2 gene expression and enhances p53 acetylation in MCF-7 cells. J. Pineal Res. 57 (1): 120–129.
123. El-Sokkary GH, Ismail IA, Saber SH (2019) Melatonin inhibits breast cancer cell invasion through modulating DJ-1/KLF17/ID-1 signaling pathway. J. Cell Biochem. 120 (3):3945–3957.
124. Czeczuga-Semeniuk E, et al. (2002) Effect of melatonin and all-trans retinoic acid on the proliferation and induction of the apoptotic pathway in the culture of human breast cancer cell line MCF-7. Pol. J. Pathol. 53 (2): 59–65.
125. Margheri M, et al. (2012) Combined effects of melatonin and all-trans retinoic acid and somatostatin on breast cancer cell proliferation and death: molecular basis for the anticancer effect of these molecules. Eur. J. Pharmacol. 681 (1–3): 34–43.
126. Soto-Vega E, Meza I, Ramírez-Rodríguez G, Benitez-King G (2004) Melatonin stimulates calmodulin phosphorylation by protein kinase C. J. Pineal Res. 37 (2): 98–106.
127. Benítez-King G, Soto-Vega E, Ramírez-Rodriguez G (2009) Melatonin modulates microfilament phenotypes in epithelial cells: implications for adhesion and inhibition of cancer cell migration. Histol. Histopathol. 24 (6): 789–799.
128. Koşar PA, Nazıroğlu M, Övey İS, Çiğ B (2016) Synergic Effects of Doxorubicin and Melatonin on Apoptosis and Mitochondrial Oxidative Stress in MCF-7 Breast Cancer Cells: Involvement of TRPV1 Channels. J. Membr. Biol. 249 (1–2): 129–140.
129. Nooshinfar E, et al. (2016) Melatonin promotes ATO-induced apoptosis in MCF-7 cells: Proposing novel therapeutic potential for breast cancer. Biomed. Pharmacother. 83: 456–465.
130. Alonso-González C, et al. (2018) Melatonin enhances the apoptotic effects and modulates the changes in gene expression induced by docetaxel in MCF-7 human breast cancer cells. Int. J. Oncol. 52 (2): 560–570.
131. Wenzel U, Nickel A, Daniel H (2005) Melatonin potentiates flavone-induced apoptosis in human colon cancer cells by increasing the level of glycolytic end products. Int. J. Cancer 116 (2): 236–242.
132. González-Puga C, et al. (2005) Selective CCK-A but not CCK-B receptor antagonists inhibit HT-29 cell proliferation: Synergism with pharmacological levels of melatonin. J. Pineal Res. 39 (3): 243–250.
133. García-Navarro A, et al. (2007) Cellular mechanisms involved in the melatonin inhibition of HT-29 human colon cancer cell proliferation in culture. J. Pineal Res. 43 (2): 195–205.
134. Pariente R, Bejarano I, Espino J, Rodríguez AB, Pariente JA (2017) Participation of MT3 melatonin receptors in the synergistic effect of melatonin on cytotoxic and apoptotic actions evoked by chemotherapeutics. Cancer Chemother. Pharmacol. 80 (5):985–998.
135. Espino J, et al. (2018) Melatonin increases the effect of 5-fluorouracil-based chemotherapy in human colorectal adenocarcinoma cells in vitro. Mol. Cell Biochem. 440 (1–2): 43–51.
136. Kontek R, Jakubczak M, Matlawska-Wasowska K (2014) The antioxidants, vitamin A and E but not vitamin C and melatonin enhance the proapoptotic effects of irinotecan in cancer cells in vitro. Toxicol. Vitr. 28 (2): 282–291.
137. Wang H, et al. (2013) Sodium arsenite induces cyclooxygenase-2 expression in human uroepithelial cells through MAPK pathway activation and reactive oxygen species induction. Toxicol. Vitr. 27 (3): 1043–1048.
138. Hong Y, et al. (2014) Melatonin treatment induces interplay of apoptosis, autophagy, and senescence in human colorectal cancer cells. J. Pineal Res. 56 (3): 264–274.
139. Batista APC, et al. (2014) Ultrastructural aspects of melatonin cytotoxicity on Caco-2 cells in vitro. Micron. 59: 17–23.
140. Zou D-B, et al. (2015) Melatonin inhibits the Migration of Colon Cancer RKO cells by Down-regulating Myosin Light Chain Kinase Expression through Cross-talk with p38 MAPK. Asian Pac. J. Cancer Prev. 16 (14): 5835–5842.
141. Yun CW, Kim S, Lee JH, Lee SH (2018) Melatonin promotes apoptosis of colorectal cancer cells via superoxide-mediated or stress by inhibiting cellular prion protein expression. Anticancer Res. 38 (7): 3951–3960.
142. Tam CHT, et al. (2010) Common polymorphisms in MTNR1B, G6PC2 and GCK are associated with increased fasting plasma glucose and impaired beta-cell function in Chinese subjects. PLoS One 5 (7): e11428.
143. Granzotto M, Rapozzi V, Decorti G, Giraldi T (2001) Effects of melatonin on doxorubicin cytotoxicity in sensitive and pleiotropically resistant tumor cells. J. Pineal Res. 31 (3):206–213.
144. Rubio S, et al. (2007) Inhibition of proliferation and induction of apoptosis by melatonin in human myeloid HL-60 cells. J. Pineal Res. 42 (2): 131–138.
145. Bejarano I, et al. (2011) Pro-oxidant effect of melatonin in tumour leucocytes: Relation with its cytotoxic and pro-apoptotic effects. Basic. Clin. Pharmacol. Toxicol. 108 (1): 14–20.
146. Krestinina O, et al. (2018) Melatonin can strengthen the effect of retinoic acid in HL-60 cells. Int. J. Mol. Sci. 19 (10): 2873.
147. Jang SS, Kim WD, Park WY (2009) Melatonin exerts differential actions on X-ray radiation-induced apoptosis in normal mice splenocytes and Jurkat leukemia cells. J. Pineal Res. 47 (2): 147–155.
148. Sánchez-Hidalgo M, Lee M, de la Lastra CA, Guerrero JM, Packham G (2012) Melatonin inhibits cell proliferation and induces caspase activation and apoptosis in human malignant lymphoid cell lines. J. Pineal Res. 53 (4): 366–373.
149. Zhelev Z, Ivanova D, Bakalova R, Aoki I, Higashi T (2017) Synergistic cytotoxicity of melatonin and new-generation anticancer drugs against leukemia lymphocytes but not normal lymphocytes. Anticancer Res. 37 (1): 149–159.
150. Büyükavci M, Özdemir Ö, Buck S, Ravindranath Y, Savaşan S (2011) Effect of melatonin on the cytotoxicity of chemotherapeutic drugs in human leukemia cells. In Vivo (Brooklyn) 25 (3): 405–409.
151. Perdomo J, et al. (2013) Melatonin induces apoptosis through a caspase-dependent but reactive oxygen species-independent mechanism in human leukemia Molt-3 cells. J. Pineal. Res. 55 (2): 195–206.
152. Quintana C, et al. (2016) Melatonin enhances hyperthermia-induced apoptotic cell death in human leukemia cells. J. Pineal Res. 61 (3): 381–395.
153. Kikuchi Y, Kita T, Miyauchi M, Iwano I, Kato K (1989) Inhibition of human ovarian cancer cell proliferation in vitro by neuroendocrine hormones. Gynecol. Oncol. 32 (1): 60–64.
154. Shellard SA, Whelan R, Hill BT (1989) Growth inhibitory and cytotoxic effects of melatonin and its metabolites on human tumour cell lines in vitro. Br. J. Cancer 60 (3): 288–290.
155. Futagami M, Sato S, Sakamoto T, Yokoyama Y, Saito Y (2001) Effects of melatonin on the proliferation and cis-diamminedichloroplatinum (CDDP) sensitivity of cultured human ovarian cancer cells. Gynecol. Oncol. 82.(3): 544–549.
156. Kim J-H, et al. (2012) Melatonin synergistically enhances cisplatin-induced apoptosis via the dephosphorylation of ERK/p90 ribosomal S6 kinase/heat shock protein 27 in SK-OV-3 cells. J. Pineal Res. 52 (2): 244–252.
157. Akbarzadeh M, et al. (2016) Effects of combination of melatonin and laser irradiation on ovarian cancer cells and endothelial lineage viability. Lasers Med. Sci. 31 (8): 1565–1572.
158. Shen CJ, Chang CC, Chen YT, Lai CS, Hsu YC (2016) Melatonin suppresses the growth of ovarian cancer cell lines (OVCAR-429 and PA-1) and potentiates the effect of G1 arrest by targeting CDKs. Int. J. Mol. Sci. 17 (2):176.
159. Zemła A, Grzegorek I, Dzięgiel P, Jabłońska K (2017) Melatonin Synergizes the Chemotherapeutic Effect of Cisplatin in Ovarian Cancer Cells Independently of MT1 Melatonin Receptors. In Vivo 31 (5): 801–809.
160. Ataei N, Aghaei M, Panjehpour M (2018) The protective role of melatonin in cadmium-induced proliferation of ovarian cancer cells. Res. Pharm. Sci. 13 (2): 159–167.
161. Fic M, et al. (2007) Effect of melatonin on cytotoxicity of doxorubicin toward selected cell lines (human keratinocytes, lung cancer cell line A-549, laryngeal cancer cell line HEp-2). In Vivo (Brooklyn) 21 (3): 513–518.
162. Kim W, Jeong JW, Kim JE (2014) CCAR2 deficiency augments genotoxic stress-induced apoptosis in the presence of melatonin in non-small cell lung cancer cells. Tumor. Biol. 35 (11): 10919–10929.
163. Fan C, et al. (2015) HDAC1 inhibition by melatonin leads to suppression of lung adenocarcinoma cells via induction of oxidative stress and activation of apoptotic pathways. J. Pineal Res. 59 (3): 321–333.
164. Lu JJ, et al. (2016) Melatonin inhibits AP-2β/hTERT, NF-κB/COX-2 and Akt/ERK and activates caspase/Cyto C signaling to enhance the antitumor activity of berberine in lung cancer cells. Oncotarget 7 (3): 2985–3001.
165. Yun M, et al. (2014) Melatonin Sensitizes H1975 Non-Small-Cell Lung Cancer Cells Harboring a T790M-Targeted Epidermal Growth Factor Receptor Mutation to the Tyrosine Kinase Inhibitor Gefitinib. Cell Physiol. Biochem. 34 (3): 865–872.
166. Plaimee P, Khamphio M, Weerapreeyakul N, Barusrux S, Johns NP (2014) Immunomodulatory effect of melatonin in SK-LU-1 human lung adenocarcinoma cells co-cultured with peripheral blood mononuclear cells. Cell Prolif. 47 (5): 406–415.
167. Plaimee P, Weerapreeyakul N, Barusrux S, Johns NP (2015) Melatonin potentiates cisplatin-induced apoptosis and cell cycle arrest in human lung adenocarcinoma cells. Cell Prolif. 48 (1): 67–77.
168. Joo SS, Yoo YM (2009) Melatonin induces apoptotic death in LNCaP cells via p38 and JNK pathways: Therapeutic implications for prostate cancer. J. Pineal Res. 47 (1): 8–14.
169. Franco DG, Moretti IF, Marie SKN (2018) Mitochondria transcription factor a: A putative target for the effect of melatonin on U87MG malignant glioma cell line. Molecules 23 (5): 1129.
170. Kocyigit A, Guler EM, Karatas E, Caglar H, Bulut H (2018) Dose-dependent proliferative and cytotoxic effects of melatonin on human epidermoid carcinoma and normal skin fibroblast cells. Mutat, Res. Genet. Toxicol. Environ. Mutagen 829–830: 50–60.
171. Zou ZW, et al. (2018) Melatonin suppresses thyroid cancer growth and overcomes radioresistance via inhibition of p65 phosphorylation and induction of ROS. Redox. Biol. 16: 226–236.
172. Song J, et al. (2018) Melatonin induces the apoptosis and inhibits the proliferation of human gastric cancer cells via blockade of the AKT/MDM2 pathway. Oncol. Rep. 39 (4):1975–1983.
173. Zhu C, Huang Q, Zhu H (2018) Melatonin Inhibits the Proliferation of Gastric Cancer Cells Through Regulating the miR-16-5p-Smad3 Pathway. DNA Cell Biol. 37 (3): 244–252.
174. Shen Y-QQ, et al. (2018) Combination of melatonin and rapamycin for head and neck cancer therapy: Suppression of AKT/mTOR pathway activation, and activation of mitophagy and apoptosis via mitochondrial function regulation. J. Pineal Res. 64 (3): e12461.
175. Halliwell B (2006) Reactive species and antioxidants. Redox biology is a fundamental theme of aerobic life. Plant Physiol. 141 (2): 312–322.
176. Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem. J. 417 (1): 1–13.
177. Lin MT, Beal MF (2006) Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443 (7113): 787–795.
178. Nunnari J, Suomalainen A (2012) Mitochondria: In sickness and in health. Cell 148 (6): 1145–1159.
179. Tan DX, Reiter RJ (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2 (1):44–66.
180. Reiter RJ, et al. (2017) Melatonin as a mitochondria-targeted antioxidant: one of evolution’s best ideas. Cell Mol. Life Sci. 74 (21): 3863–3881.
181. Suofu Y, et al. (2017) Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. USA 114 (38): E7997–E8006.
182. Wang L, et al. (2017) Plant mitochondria synthesize melatonin and enhance the tolerance of plants to drought stress. J. Pineal Res. 63 (3): e12429.
183. He C, et al. (2016) Mitochondria synthesize melatonin to ameliorate its function and improve mice oocyte’s quality under in vitro conditions. Int. J. Mol. Sci. 17 (6):939.
184. Yang M, et al. (2019) AANAT knockdown and melatonin supplementation in embryo development: involvement of mitochondrial function and dna methylation. Antioxidants Redox. Signal. 30 (18): 2050–2065.
185. Zheng X, et al. (2017) Chloroplastic biosynthesis of melatonin and its involvement in protection of plants from salt stress. Sci. Rep. 7 (1): 41236.
186. Sainz RM, et al. (2003) Melatonin and cell death: Differential actions on apoptosis in normal and cancer cells. Cell Mol. Life Sci. 60 (7): 1407–1426.
187. Lee CS, Park SY, Ko HH, Han ES (2004) Effect of change in cellular GSH levels on mitochondrial damage and cell viability loss due to mitomycin c in small cell lung cancer cells. Biochem. Pharmacol. 68 (9): 1857–1867.
188. Song N, et al. (2012) Melatonin suppresses doxorubicin-induced premature senescence of A549 lung cancer cells by ameliorating mitochondrial dysfunction. J. Pineal Res. 53 (4): 335–343.
189. Delbridge ARD, Strasser A (2015) The BCL-2 protein family, BH3-mimetics and cancer therapy. Cell Death Differ. 22 (7): 1071–1080.
190. Kong H, Chandel NS (2018) Regulation of redox balance in cancer and T cells. J. Biol. Chem. 293 (20): 7499–7507.
191. Proietti S, Cucina A, Minini M, Bizzarri M (2017) Melatonin, mitochondria, and the cancer cell. Cell Mol. Life Sci. 74 (21): 4015–4025.
192. de Almeida Chuffa LG, et al. (2019) Mitochondrial functions and melatonin: a tour of the reproductive cancers. Cell Mol. Life Sci. 76 (5): 837–863.
193. Hevia D, et al. (2017) Melatonin decreases glucose metabolism in prostate cancer cells: A 13C stable isotope-resolved metabolomic study. Int. J. Mol. Sci. 18 (8): 1620.
194. Mao L, et al. (2016) Melatonin suppression of aerobic glycolysis (Warburg effect), survival signalling and metastasis in human leiomyosarcoma. J. Pineal Res. 60 (2): 167–177.
195. Yu Z, et al. (2018) Mitochondrial cytochrome P450 (CYP) 1B1 is responsible for melatonin-induced apoptosis in neural cancer cells. J. Pineal Res. 65 (1): e12478.
196. Waseem M, et al. (2017) Melatonin pre-treatment mitigates SHSY-5Y cells against oxaliplatin induced mitochondrial stress and apoptotic cell death. PLoS One 12 (7): e0180953.
197. Huo X, et al. (2017) Human transporters, PEPT1/2, facilitate melatonin transportation into mitochondria of cancer cells: An implication of the therapeutic potential. J. Pineal Res. 62 (4): e12390.
198. Mayo JC, et al. (2017) IGFBP3 and MAPK/ERK signaling mediates melatonin-induced antitumor activity in prostate cancer. J. Pineal Res. 62 (1): 1–17.
199. Yang CY, et al. (2017) Melatonin exerts anti-oral cancer effect via suppressing LSD1 in patient-derived tumor xenograft models. Oncotarget 8 (20): 33756–33769.
200. Cavallo F, De Giovanni C, Nanni P, Forni G, Lollini PL (2011) 2011: The immune hallmarks of cancer. Cancer Immunol. Immunother. 60 (3): 319–326.
201. Hanahan D, Weinberg RA (2011) Hallmarks of cancer: The next generation. Cell 144 (5): 646–674.
202. Weinhouse S, Warburg O, Burk D, Schade AL (1956) On respiratory impairment in cancer cells. Science 124 (3215): 267–272.
203. Warburg O (1964) Prefatory Chapter. Annu. Rev. Biochem. 33 (1): 1–15.
204. Pavlova NN, Thompson CB (2016) The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 23 (1): 27–47.
205. Thompson CB (2011) Rethinking the regulation of cellular metabolism. Cold Spring Harb Symp. Quant. Biol. 76: 23–29.
206. Barthel A, et al. (1999) Regulation of GLUT1 gene transcription by the serine/threonine kinase AKT1. J. Biol. Chem. 274 (29): 20281–20286.
207. Murakami T, et al. (1992) Identification of two enhancer elements in the gene encoding the type 1 glucose transporter from the mouse which are responsive to serum, growth factor, and oncogenes. J. Biol. Chem. 267 (13): 9300–9306.
208. Wang R, et al. (2011) The Transcription Factor Myc Controls Metabolic Reprogramming upon T Lymphocyte Activation. Immunity 35 (6): 871–882.
209. Reynolds MR, et al. (2014) Control of glutamine metabolism by the tumor suppressor Rb. Oncogene 33 (5): 556–566.
210. Koppenol WH, Bounds PL, Dang C V. (2011) Otto Warburg’s contributions to current concepts of cancer metabolism. Nat. Rev. Cancer 11 (5): 325–337.
211. Warburg O (1956) On the origin of cancer cells. Science 123 (3191): 309–314.
212. Heiden MG Vander, Cantley LC, Thompson CB (2009) Understanding the warburg effect: The metabolic requirements of cell proliferation. Science 324 (5930):1029–1033.
213. DeBerardinis RJ, Lum JJ, Hatzivassiliou G, Thompson CB (2008) The Biology of cancer: metabolic reprogramming fuels cell growth and proliferation. Cell Metab. 7 (1): 11–20.
214. Ward PS, Thompson CB (2012) Metabolic reprogramming: a cancer hallmark even Warburg did not anticipate. Cancer Cell 21 (3): 297–308.
215. Wellen KE, Thompson CB (2012) A two-way street: Reciprocal regulation of metabolism and signalling. Nat. Rev. Mol. Cell Biol. 13 (4): 270–276.
216. Dauchy RT, et al. (2014) Circadian and melatonin disruption by exposure to light at night drives intrinsic resistance to tamoxifen therapy in breast cancer. Cancer Res. 74 (15): 4099–4110.
217. Xiang S, et al. (2015) Doxorubicin resistance in breast cancer is driven by light at night-induced disruption of the circadian melatonin signal. J. Pineal Res. 59 (1): 60–69.
218. Sanchez-Sanchez AM, et al. (2015) Melatonin cytotoxicity is associated to Warburg effect inhibition in Ewing sarcoma cells. PLoS One 10 (8): e0135420.
219. Gobbo MG, et al. (2015) Influence of melatonin on the proliferative and apoptotic responses of the prostate under normal and hyperglycemic conditions. J. Diabetes Res. 2015: 538529.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.