Functional interplay of melatonin in the bile duct and gastrointestinal tract to mitigate disease development: An overview
Biliary and gastrointestinal melatonin
Abstract
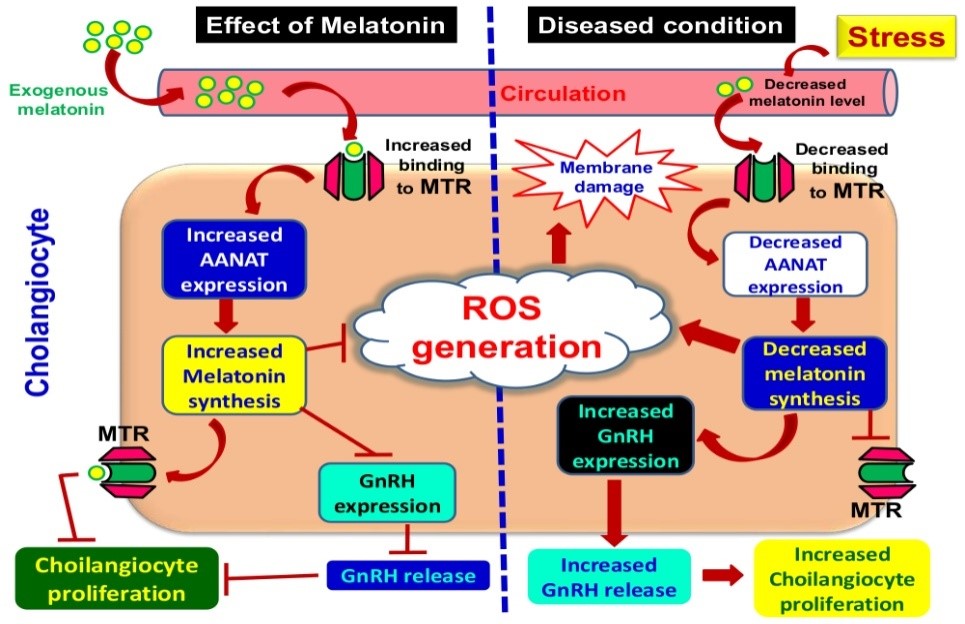
Prevalence of bile duct and gastrointestinal (GI) tract associated diseases is increasing globally. Commonly, the bile duct epithelial cell (cholangiocytes) malfunction and its uncontrolled proliferation often cause liver fibrosis and tumorigenesis, particularly the cholangiocarcinoma. Specifically, GI tract is constantly under diverse endogenous and exogenous stressors which interrupt GI physiological functions and promote inflammation, tissue damage, ulceration, gastrointestinal bleeding, gastroesophageal reflux disease (GERD), irritable bowel disease (IBD) and gastritis. On the other hand, melatonin exhibits important functions in both cholangiocyte and GI tract. The abundance of melatonin generated in the GI tract and its widely distributed receptors facilitate its protective effects in GI tissues. In the most of the cases, the disease progression in GI tract, particularly in bile duct, is associated with endogenous melatonergic system suppression. Therefore, to increase the endogenous melatonin production appears a suitable strategy to retard the disease development in these tissues. Melatonin administration or, exposure to prolonged darkness not only reverse the detrimental biochemical alterations, but also inhibit cholangiocyte proliferation as well as ulceration in the GI tract. Thus, use of melatonin as a natural therapeutic agent is beneficial and exhibits advantages over other contemporary drugs in prevention and treatment of bile duct and gastrointestinal tract associated diseases.
References
2. Pollheimer MJ, Fickert P, Stieger B (2014) Chronic cholestatic liver diseases: clues from histopathology for pathogenesis. Mol. Aspects Med. 37: 35-56. doi: 10.1016/j.mam.2013. 10.001.
3. Alpini G, McGill JM, Larusso NF (2002) The pathobiology of biliary epithelia. Hepatology 35: 1256–1268. doi:10.1053/jhep.2002.33541.
4. Williams MJ, Clouston AD, Forbes SJ (2014) Links between hepatic fibrosis, ductular reaction, and progenitor cell expansion. Gastroenterology 146: 349–356. doi:10.1053/j.gastro.2013.11.034.
5. Lazaridis KN, Strazzabosco M, Larusso NF (2004) The cholangiopathies: disorders of biliary epithelia. Gastroenterology 127: 1565–1577. doi:10.1053/j.gastro.2004.08.006.
6. Franchitto A, Onori P, Renzi A, et al. (2013) Recent advances on the mechanisms regulating cholangiocyte proliferation and the significance of the neuroendocrine regulation of cholangiocyte pathophysiology. Ann. Transl. Med. 1: 27. doi:10.3978/ j.issn.2305-5839.2012.10.03.
7. Maroni L, Haibo B, Ray D, et al. (2015) Functional and structural features of cholangiocytes in health and disease. Cell. Mol. Gastroenterol. Hepatol. 1: 368–380. doi:10.1016/j.jcmgh.2015.05.005.
8. Bhattacharyya A, Chattopadhyay R, Mitra S, et al. (2014) Oxidative stress: an essential factor in the pathogenesis of gastrointestinal mucosal diseases. Physiol. Rev. 94: 329–354. doi:10.1152/physrev.00040.2012.
9. Zalups RK (2000) Molecular interactions with mercury in the kidney. Pharmacol. Rev. 52: 113-143.
10. Koh DH, Bhatti P, Coble JB, et al. (2014) Calibrating a population-based job-exposure matrix using inspection measurements to estimate historical occupational exposure to lead for a population-based cohort in Shanghai, China. J. Exp. Sci. Env. Epid. 24: 9–16. doi: 10.1038/jes.2012.86.
11. Victoni T, Coelho FR, Soares AL, et al. (2010) Local and remote tissue injury upon intestinal ischemia and reperfusion depends on the TLR/MyD88 signaling pathway. Med. Microbiol. Immunol. 199: 35–42.
12. Beckman JS, Koppenol WH (1996) Nitric oxide, superoxide and peroxynitrite: the good, the bad and the ugly. Am. J. Physiol. 271: C1424–C1437. doi: 10.1152/ajpcell.1996. 271.5.c1424.
13. Pal PK, Bhattacharjee B, Chattopadhyay A, et al. (2019) Melatonin as an armament against non-steroidal anti-inflammatory drug (NSAID) induced gastric injury: An overview. Melatonin Res. 2: 116-138. doi: 10.32794/mr11250015.
14. Wongrakpanich S, Wongrakpanich A, Melhado K, et al. (2018) A comprehensive review of non-steroidal anti-inflammatory drug use in the elderly. Aging Dis. 9: 143-150. http://dx.doi.org/10.14336/AD.2017.0306.
15. Fritsche KL (2015) The science of fatty acids and inflammation. Adv. Nutr. 6: 293S–301S. doi: 10.3945/an.114.006940.
16. Wild CP, Hardie LJ (2003) Reflux, Barrett’s oesophagus and adenocarcinoma: burning questions. Nat. Rev. Cancer 3: 676–684.
17. Song S, Guha S, Liu K, et al. (2007) COX-2 induction by unconjugated bile acids involves reactive oxygen species-mediated signalling pathways in Barrett’s oesophagus and oesophageal adenocarcinoma. Gut 56: 1512–1521.doi: 10.1136/gut.2007.121244.
18. DeMorrow S, Francis H, Gaudio E, et al. (2008) The endocannabinoid anandamide inhibits cholangiocarcinoma growth via activation of the noncanonical Wnt signaling pathway. Am. J. Physiol. Gastrointest. Liver Physiol. 295: G1150–G1158. doi:10.1152/ajpgi.90455.2008.
19. Marzioni M, Glaser S, Francis H, et al. (2004) Autocrine/paracrine regulation of the growth of the biliary tree by the neuroendocrine hormone serotonin. Gastroenterology 128: 121–137. doi:10.1053/j.gastro.2004.10.002.
20. Renzi A, Glaser S, Demorrow S, et al. (2011) Melatonin inhibits cholangiocyte hyperplasia in cholestatic rats by interaction with MT1 but not MT2 melatonin receptors. Am. J. Physiol. Gastrointest. Liver. Physiol. 301: G634–G643. doi:10.1152/ajpgi.00206. 2011.
21. Tan DX, Chen LD, Poeggeler B, et al. (1993) Melatonin: a potent, endogenous hydroxyl radical scavenger. Endocr. J. 1:57–60.
22. Rodriguez C, Mayo JC, Sainz RM, et al. (2004) Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 36: 1–9.
23. Pal PK, Hasan NK, Maitra SK (2016) Gut melatonin response to microbial infection in carp Catla catla. Fish Physiol. Biochem. 42: 579–592. doi: 10.1007/s10695-015-0161-7.
24. Pal PK, Maitra SK (2018) Response of gastrointestinal melatonin, antioxidants, and digestive enzymes to altered feeding conditions in carp (Catla catla). Fish Physiol. Biochem. 44: 1061-1073. https://doi.org/10.1007/s10695-018-0494-0.
25. Pal PK, Bhattacharjee B, Ghosh A, et al. (2019) Adrenaline induced disruption of endogenous melatonergic system, antioxidant and inflammatory responses in the gastrointestinal tissues of male Wistar rat: an in vitro study. Melatonin Res. 1: 109–131. doi: 10.32794/mr11250007.
26. Pal PK, Bhattacharjee B, Chattopadhyay A, et al. (2019) Pleiotropic roles of melatonin against oxidative stress mediated tissue injury in the gastrointestinal tract: An overview. Melatonin Res. 2: 158-184. DOI: 10.32794/mr11250027.
27. Tan DX, Manchester LC, Reiter RJ, et al. (1999) High physiological levels of melatonin in the bile of mammals. Life Sci. 65 (23): 2523-2529.
28. Raikhlin NT, Kvetnoy IM (1974) Lightening effect of the extract of human appendix mucosa on frog skin melanophores. Bull. Exp. Biol. Med. 8: 114–116.
29. Bubenik GA (1999) Localization and physiological significance of gastrointestinal melatonin. In: R Watson (eds.) Melatonin in health promotion. CRC press, Boca Raton, Florida, pp. 21–39.
30. Chen CQ, Fichna J, Bashashati M, et al. (2011) Distribution, function and physiological role of melatonin in the lower gut. World J. Gastroenterol. 17: 3888-3898. doi: 10.3748/wjg.v17.i34.3888.
31. Nathanson MH, Boyer JL (1991) Mechanisms and regulation of bile secretion. Hepatology 14: 551-566.
32. Kanno N, LeSage G, Glaser S, et al. (2000) Functional heterogeneity of the intrahepatic biliary epithelium. Hepatology 31: 555-561.
33. Ludwig J (1987) New concepts in biliary cirrhosis. Semin. Liver Dis.7: 293-301.
34. Alpini G, Roberts S, Kuntz SM, et al. (1996) Morphological, molecular, and functional heterogeneity of cholangiocytes from normal rat liver. Gastroenterology 110: 1636-1643. doi: 10.1053/gast.1996.v110.pm8613073.
35. Alpini G, Glaser S, Robertson W, et al. (1997) Large but not small intrahepatic bile ducts are involved in secretin-regulated ductal bile secretion. Am. J. Physiol. 272: G1064-G1074. doi: 10.1152/ajpgi.1997.272.5.G1064.
36. Glaser SS, Gaudio E, Rao A, et al. (2009) Morphological and functional heterogeneity of the mouse intrahepatic biliary epithelium. Lab. Invest. 89: 456-469. doi: 10.1038/labinvest.2009.6.
37. Gaudio E, Onori P, Pannarale L, et al. (1996) Hepatic microcirculation and peribiliary plexus in experimental biliary cirrhosis: a morphological study. Gastroenterology 111: 1118-124. doi: 10.1016/s0016-5085(96)70081-1.
38. Gaudio E, Barbaro B, Alvaro D, et al. (2006) Administration of r-VEGF-A prevents hepatic artery ligation-induced bile duct damage in bile duct ligated rats. Am. J. Physiol. Gastrointest. Liver. Physiol. 291: G307-G317. doi: 10.1152/ajpgi.00507.2005.
39. Terada T, Ishida F, Nakanuma Y (1989) Vascular plexus around intrahepatic bile ducts in normal livers and portal hypertension. J. Hepatol. 8: 139-149. doi: 10.1016/0168-8278(89)90001-9.
40. Alpini G, Lenzi R, Sarkozi L, et al. (1988) Biliary physiology in rats with bile ductular cell hyperplasia. Evidence for a secretory function of proliferated bile ductules. J. Clin. Invest. 81: 569-578. doi: 10.1172/JCI113355.
41. Kanno N, LeSage G, Glaser S, et al. (2001) Regulation of cholangiocyte bicarbonate secretion. Am. J. Physiol. Gastrointest. Liver. Physiol. 281: G612-G625. doi: 10.1152/ajpgi.2001.281.3.G612.
42. Tietz PS, Alpini G, Pham LD, et al. (1995) Somatostatin inhibits secretin-induced ductal hypercholeresis and exocytosis by cholangiocytes. Am. J. Physiol. 269: G110-G118. doi: 10.1152/ajpgi.1995.269.1.G110.
43. Alvaro D, Alpini G, Jezequel AM, et al. (1997) Role and mechanisms of action of acetylcholine in the regulation of rat cholangiocyte secretory functions. J. Clin. Invest. 100: 1349-1362. doi: 10.1172/JCI119655.
44. LeSage GD, Alvaro D, Glaser S, et al. (2004) Alpha-1 adrenergic receptor agonists modulate ductal secretion of BDL rats via Ca(2+)- and PKC-dependent stimulation of cAMP. Hepatology 40: 1116-1127. doi: 10.1002/hep.20424.
45. Glaser S, Alvaro D, Francis H, et al. (2006) Adrenergic receptor agonists prevent bile duct injury induced by adrenergic denervation by increased cAMP levels and activation of Akt. Am. J. Physiol. Gastrointest. Liver Physiol. 290: G813-G826. doi: 10.1152/ajpgi.00306.2005.
46. Han Y, Glaser S, Meng F, et al. (2013) Recent advances in the morphological and functional heterogeneity of the biliary epithelium. Exp. Biol. Med. (Maywood) 238: 549-565. doi: 10.1177/1535370213489926.
47. Banales JM, Arenas F, Rodríguez-Ortigosa CM, et al. (2006) Bicarbonate-rich choleresis induced by secretin in normal rat is taurocholate-dependent and involves AE2 anion exchanger. Hepatology 43: 266-275. doi: 10.1002/hep.21042.
48. LeSage GD, Glaser SS, Marucci L, et al. (1999) Acute carbon tetrachloride feeding induces damage of large but not small cholangiocytes from BDL rat liver. Am. J. Physiol. 276: G1289-G1301. doi: 10.1152/ajpgi.1999.276.5.G1289.
49. Lanzini A (2003) Bile. In: Trugo L and Finglas PM (Eds.) Encyclopedia of food sciences and nutrition (2nd edition). pp. 471-478. https://doi.org/10.1016/B0-12-227055-X/00095-X.
50. Alpini G, Ulrich CD, 2nd, Phillips JO, et al. (1994) Upregulation of secretin receptor gene expression in rat cholangiocytes after bile duct ligation. Am. J. Physiol. Gastrointest. Liver Physiol. 266: G922-G928. doi: 10.1152/ajpgi.1994.266.5.G922.
51. Gigliozzi A, Alpini G, Baroni GS, et al. (2004) Nerve growth factor modulates the proliferative capacity of the intrahepatic biliary epithelium in experimental cholestasis. Gastroenterology 127: 1198–1209. doi:10.1053/j.gastro.2004.06.023.
52. Alvaro D, Mancino MG, Glaser S, et al. (2007) Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology 132: 415-431. https://doi.org/10.1053/j.gastro.2006.07.023.
53. Mancinelli R, Onori P, Gaudio E, et al. (2009) Follicle-stimulating hormone increases cholangiocyte proliferation by an autocrine mechanism via cAMP-dependent phosphorylation of ERK1/2 and Elk-1. Am. J. Physiol. Gastrointest. Liver Physiol. 297: G11-G26. doi: 10.1152/ajpgi.00025.2009.
54. Glaser S, Lam IP, Franchitto A, et al. (2010) Knockout of secretin receptor reduces large cholangiocyte hyperplasia in mice with extrahepatic cholestasis induced by bile duct ligation. Hepatology 52: 204–214. doi:10.1002/hep.23657.
55. Francis HL, Demorrow S, Franchitto A, et al. (2012) Histamine stimulates the proliferation of small and large cholangiocytes by activation of both IP3/Ca2+ and cAMP-dependent signaling mechanisms. Lab. Invest. 92: 282–294. doi:10.1038/ labinvest.2011.158.
56. Quinn M, Ueno Y, Pae HY, et al. (2012) Suppression of the HPA axis during extrahepatic biliary obstruction induces cholangiocyte proliferation in the rat. Am. J. Physiol. Gastrointest. Liver Physiol. 302: G182–G193. doi:10.1152/ajpgi.00205.2011.
57. McMillin M, Frampton G, Quinn M, et al. (2015) Suppression of the HPA axis during cholestasis can be attributed to hypothalamic bile acid signaling. Mol. Endocrinol. 29: 1720–1730. doi:10.1210/me.2015-1087.
58. Ray D, Han Y, Franchitto A, et al. (2015) Gonadotropin-releasing hormone stimulates biliary proliferation by paracrine/autocrine mechanisms. Am. J. Pathol. 185: 1061– 1072. doi:10.1016/j.ajpath.2014.12.004.
59. Roy D, Belsham DD (2002) Melatonin receptor activation regulates GnRH gene expression and secretion in GT1-7GnRH neurons. Signal transduction mechanisms. J. Biol. Chem. 277: 251–258. doi:10.1074/ jbc.M108890200.
60. Schomerus C, Korf HW (2005) Mechanisms regulating melatonin synthesis in the mammalian pineal organ. Ann. NY. Acad. Sci. 1057: 372–383. doi:10.1196/annals. 1356.028.
61. Mancinelli R, Franchitto A, Gaudio E, et al. (2010) After damage of large bile ducts by gamma-aminobutyric acid, small ducts replenish the biliary tree by amplification of calcium-dependent signaling and de novo acquisition of large cholangiocyte phenotypes. Am. J. Pathol. 176: 1790-1800. https://doi.org/10.2353/ajpath.2010.090677.
62. Marzioni M, Saccomanno S, Candelaresi C, et al. (2010) Pancreatic Duodenal Homeobox-1 de novo expression drives cholangiocyte neuroendocrine-like trans differentiation. J. Hepatol. 53: 663–670. doi:10.1016/j.jhep.2010.04.022.
63. Sato K, Meng F, Giang T, et al. (2018) Mechanisms of cholangiocyte responses to injury. Biochim. Biophys. Acta Mol. Basis Dis. 1864: 1262-1269. doi: 10.1016/j.bbadis.2017.06.017.
64. Francis H, Franchitto A, Ueno Y, et al. (2007) H3 histamine receptor agonist inhibits biliary growth of BDL rats by downregulation of the cAMP-dependent PKA/ ERK1/2/ELK-1 pathway. Lab. Invest. 87: 473–487. https://doi.org/10.1038/labinvest. 3700533.
65. Francis H, Glaser S, DeMorrow S, et al. (2008) Small mouse cholangiocytes proliferate in response to H1 histamine receptor stimulation by activation of the IP3/CAMK I/CREB pathway. Am. J. Physiol. Cell. Physiol. 295: C499–C513. doi: 10.1152/ajpcell. 00369.2007.
66. Francis H, Onori P, Gaudio E, et al. (2009) H3 histamine receptor mediated activation of protein kinase C alpha inhibits the growth of cholangiocarcinoma in vitro and in vivo. Mol. Cancer Res. 7: 1704–1713. doi: 10.1158/1541-7786.MCR-09-0261.
67. Meng F, Han Y, Staloch D, et al. (2011) The H4HR agonist, clobenpropit, suppresses human cholangiocarcinoma progression by disruption of EMT and tumor metastasis. Hepatology. 54 (5): 1718-1728. doi: 10.1002/hep.24573.
68. Gaudio E, Barbaro B, Alvaro D, et al. (2006) Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology. 130 (4): 1270-1282. doi: 10.1053/j.gastro.2005.12.034.
69. Alvaro D, Alpini G, Onori P, et al. (2000) Estrogens stimulate proliferation of intrahepatic biliary epithelium in rats. Gastroenterology 119 (6): 1681-1691. https://doi.org/10.1053/gast.2000.20184.
70. Glaser S, DeMorrow S, Francis H (2008) Progesterone stimulates the proliferation of female and male cholangiocytes via autocrine/paracrine mechanisms. Am. J. Physiol. Gastrointest. Liver Physiol. 295 (1): G124–G136. doi: 10.1152/ajpgi.00536.2007.
71. Mancinelli R, Franchitto A, Glaser S, et al. (2013) GABA induces the differentiation of small into large cholangiocytes by activation of Ca(2+) /CaMK I-dependent adenylyl cyclase 8. Hepatology 58: 251-263. doi: 10.1002/hep.26308.
72. Chapman R, Fevery J, Kalloo A, et al. (2010) Diagnosis and management of primary sclerosing cholangitis. Hepatology 51: 660-678. https://doi.org/10.1002/hep.23294.
73. Lindor KD, Bowlus CL, Boyer J, et al. (2019) Primary biliary cholangitis: 2018 Practice guidance from the american association for the study of liver diseases. Hepatology 69: 394-419. https://doi.org/10.1002/hep.30145.
74. Carpino G, Cardinale V, Folseraas T, et al. (2018) Hepatic stem/progenitor cell activation differs between primary sclerosing and primary biliary cholangitis. Am. J. Pathol. 188: 627-639. doi: 10.1016/j.ajpath.2017.11.010.
75. Sato K, Marzioni M, Meng F, et al. (2019) Ductular reaction in liver diseases: pathological mechanisms and translational significances. Hepatology 69: 420-430. doi: 10.1002/hep.30150.
76. Wu N, Kyritsi K, Invernizzi P, et al. (2017) Differential impact of MT1 and MT2 melatonin receptor deletion on biliary proliferation, senescence, and liver fibrosis duringcholestatic liver injury. Hepatology 66: A330.
77. Mekjian HS, Phillips SF, Hofmann AF (1971) Colonic secretion of water and electrolytes induced by bile acids: perfusion studies in man. J. Clin. Invest. 50: 1569–1577. doi: 10.1172/JCI106644.
78. Xu S, Pi H, Zhang L, et al. (2016) Melatonin prevents abnormal mitochondrial dynamics resulting from the neurotoxicity of cadmium by blocking calcium-dependent translocation of Drp1 to the mitochondria. J. Pineal Res. 60: 291-302. doi: 10.1111/jpi.12310.
79. Perez MJ, Briz O (2009) Bile-acid-induced cell injury and protection. World J. Gastroenterol. 15(14): 1677-1689. doi: 10.3748/wjg.15.1677.
80. Chen Y, Lv L, Jiang Z, et al. (2013) Mitofusin 2 protects hepatocyte mitochondrial function from damage induced by GCDCA. PLoS One 8 (6): e65455. https://doi.org/10.1371/journal.pone.0065455.
81. Pal PK, Hasan NK, Maitra SK (2016) Temporal relationship between the daily profiles of gut melatonin, oxidative status and major digestive enzymes in carp Catla catla. Biol. Rhythm Res. 47: 755–771. doi: 10.1080/09291016.2016.1191697.
82. Liu X, Wu W-K, Yu L, et al. (2008) Epinephrine stimulates esophageal squamous-cell carcinoma cell proliferation via beta adrenoceptor-dependent transactivation of extracellular signal-regulated kinase/cyclooxygenase-2 pathway. J. Cell Biochem. 105: 53–60. DOI: 10.1002/jcb.21802.
83. Yao H, Duan Z, Wang M, et al. (2009) Adrenaline induces chemoresistance in HT-29 colon adenocarcinoma cells. Cancer Genet. Cytogenet. 190: 81–87. doi: 10.1016/j.cancergencyto.2008.12.009.
84. Rudra S, Mukherjee D, Dutta M, et al. (2014) Orally administered melatonin protects against adrenaline-induced oxidative stress in rat liver and heart: Involvement of antioxidant mechanism(s). J. Pharm. Res. 8: 303–320. http://jprsolutions.info/files/final-file-56bff9adee9ad8.28733292.pdf.
85. Langford NJ, Ferner RE (1999) Toxicity of mercury. J. Hum. Hypertens. 13: 651–656. https://doi.org/10.1038/sj.jhh.1000896.
86. Shi H, Shi X, Liu KJ (2004) Oxidative mechanism of arsenic toxicity and carcinogenesis. Mol. Cell Biochem. 255: 67-78.
87. Barnes JL, McDowell EM, McNeil JS (1980) Studies on the pathophysiology of acute renal failure. V. Effect of chronic saline loading on the progression of proximal tubular injury and functional impairment following administration of mercuric chloride in the rat. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 32: 233–260.
88. Henning SJ, Leeper LL (1984) Duodenal uptake of lead by suckling and weanling rats. Bioi. Neonate 46: 27-35. doi: 10.1159/000242029.
89. Conrad ME, Barton JC (1978) Factors affecting the absorption and excretion of lead in the rat. Gastroenterol. 74: 731-740. doi: https://doi.org/10.1016/0016-5085(78)90253-6.
90. Valko M, Morris H, Cronin MTD (2005) Metals, toxicity and oxidative stress. Curr. Med. Chem. 12: 1161–1208. doi: 10.2174/0929867053764635.
91. Awtry EH, Loscalzo J (2000) Cardiovascular drugs. aspirin. Circulation 101: 1206-1218.
92. Yoshikawa T, Naito Y, Kishi A, et al. (1993) Role of active oxygen, lipid peroxidation, and antioxidants in the pathogenesis of gastric mucosal injury induced by indomethacin in rats. Gut 34: 732-737. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374252.
93. Brzozowski T, Konturek PC, Konturek SJ, et al. (1997) The role of melatonin and L-tryptophan in prevention of acute gastric lesions induced by stress, ethanol, ischemia, and aspirin. J. Pineal Res. 23: 79-89. https://doi.org/10.1111/j.1600-079X.1997. tb00339.x.
94. Banerjee RK (1990) Nonsteroidal anti-inflammatory drugs inhibit gastric peroxidase activity. Biochim. Biophys. Acta 1034: 275-280.
95. Das D, Bandyopadhyay D, Bhattacharjee M, et al. (1997) Hydroxyl radical is the major causative factor in stress-induced gastric ulceration. Free Radic. Biol. Med. 23: 8-18. https://doi.org/10.1016/S0891-5849(96)00547-3.
96. Naito Y, Yoshikawa T (2006) Oxidative stress Involvement and gene expression in indomethacin-induced gastropathy. Redox Rep. 11: 243–253. doi: 10.1179/135100006X 155021.
97. Tan DX, Reiter RJ (2019) Mitochondria: the birth place, battle ground and the site of melatonin metabolism in cells. Melatonin Res. 2: 44-66. doi: https://doi.org/10.32794/ mr11250011.
98. Bandyopadhyay D, Biswas K, Bandyopadhyay U, et al. (2000) Melatonin protects against stress-induced lesions by scavenging the hydroxyl radical. J. Pineal Res. 29: 143–151.
99. Chattopadhyay I, Bandyopadhyay U, Biswas K, et al. (2006) Indomethacin inactivates gastric peroxidase to induce reactive-oxygen-mediated gastric mucosal injury and curcumin protects it by preventing peroxidise inactivation and scavenging reactive oxygen. Free Radic. Biol. Med. 40: 1397–1408. doi: 10.1016/j.freeradbiomed.2005. 12.016.
100. Phull PS, Green CJ, Jacyna MR (1995) A radical view of the stomach: the role of oxygen-derived free radicals and anti-oxidants in gastroduodenal disease. Eur. J. Gastroenterol. Hepatol. 7: 265–274.
101. Mallick IH, Yang W, Winslet MC, et al. (2004) Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig. Dis. Sci. 49: 1359–1377.
102. Jarry A, Bach-Ngohou K, Masson D, et al. (2006) Human colonic myocytes are involved in post-ischemic inflammation through ADAM17-dependent TNF alpha production. Br. J. Pharmacol. 147: 64–72. doi: 10.1038/sj.bjp.0706449.
103. de La Serre CB, Ellis CL, Lee J, et al. (2010) Propensity to high-fat diet induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 299: G440–G448. doi: 10.1152/ajpgi.00098.2010.
104. Schnabl B, Brenner DA (2014) Interactions between the intestinal microbiome and liver diseases. Gastroenterol. 146: 1513–1524. doi: 10.1053/j.gastro.2014.01.020.
105. O’Hara AM, Bhattacharya A, Bai J, et al. (2006) Interleukin-8 induction by Helicobacter pylori in human gastric epithelial cells is dependent on a purinic/ apyrimidinic endonuclease-1/redoxfactor-1. J. Immunol. 177: 7990–7999.
106. Ding SZ, Minohara Y, Fan XJ, et al. (2007) Helicobacter pylori infection induces oxidative stress and programmed cell death in human gastric epithelial cells. Infect. Immun. 75: 4030–4039. doi: 10.1128/IAI.00172-07.
107. Davies GR, Simmonds NJ, Stevens TR, et al. (1992) Mucosal reactive oxygen metabolite production in duodenal ulcer disease. Gut 33: 1467–1472. doi: 10.1136/gut.33.11.1467.
108. Chen L, Zhou T, Wu N, et al. (2019) Pinealectomy or light exposure exacerbates biliary damage and liver fibrosis in cholestatic rats through decreased melatonin synthesis. Biochim. Biophys. Acta Mol. Basis. Dis. 1865: 1525-1539. doi: 10.1016/j.bbadis. 2019.03.002.
109. Reiter RJ, Mayo JC, Tan DX, et al. (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61: 253–278. doi: 10.1111/jpi.12360.
110. Galano A, Tan DX, Reiter RJ (2018) Melatonin: a versatile protector against oxidative DNA damage. Molecules 27: 23. doi: 10.3390/molecules23030530.
111. Dobocovich M, Mankowsha M (2005) Functional MP1 and MP2 melatonin receptors in mammals. Endocrine 27: 101–110. doi: 10.1385/ENDO:27:2:101.
112. Tan DX, Manchester LC, Terron MP, et al. (2007) One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 42 (1): 28-42. DOI: 10.1111/j.1600-079X.2006.00407.x.
113. Li Y, Yang Y, Feng Y, et al. (2014) A review of melatonin in hepatic ischemia/reperfusion injury and clinical liver disease. Ann. Med. 46(7): 503-511. doi: 10.3109/07853890.2014.934275.
114. Guo P, Pi H, Xu S, et al. (2014) Melatonin Improves mitochondrial function by promoting MT1/SIRT1/PGC-1 alpha-dependent mitochondrial biogenesis in cadmium-induced hepatotoxicity in vitro. Toxicol. Sci.142 (1):182-195. doi: 10.1093/toxsci/ kfu164.
115. Mitra E, Bhattacharjee B, Pal PK, et al. (2019) Melatonin protects against cadmium-induced oxidative damage in different tissues of rat: a mechanistic insight. Melatonin Res. 2: 1-21. doi: 10.32794/mr11250018.
116. Chen Y, Qing W, Sun M, et al. (2015) Melatonin protects hepatocytes against bile acid-induced mitochondrial oxidative stress via the AMPK-SIRT3-SOD2 pathway. Free Radic. Res. 49: 1275-1284. doi: 10.3109/10715762.2015.1067806.
117. Reiter RJ, Rosales-Corral SA, Manchester LC, et al. (2014) Melatonin in the biliary tract and liver: health implications. Curr. Pharm. Des. 20 (30): 4788-4801.
118. Tahan G, Akin H, Aydogan F, et al. (2010) Melatonin ameliorates liver fibrosis induced by bile-duct ligation in rats. Can. J. Surg. 53 (5): 313-318.
119. Pandi-Perumal SR, Srinivasan V, Maestroni GJ, et al. (2006) Melatonin: Nature's most versatile biological signal? FEBS J. 273: 2813–2838. doi: 10.1111/j.1742-4658.2006.05322.x.
120. Tan DX, Manchester LC, Reiter RJ, et al. (1998) Ischemia/reperfusion‐induced arrhythmias in the isolated rat heart: Prevention by melatonin. J. Pineal Res. 25: 184-191. https://doi.org/10.1111/j.1600-079X.1998.tb00558.x.
121. Ressmeyer AR, Mayo JC, Zelosko V, et al. (2003) Antioxidant properties of the melatonin metabolite N1-acetyl-5-methoxykynuramine (AMK): scavenging of free radicals and prevention of protein destruction. Redox Rep. 8 (4): 205-213. doi: 10.1179/135100003225002709.
122. Chojnacki C, Walecka-Kapica E, Klupińska G, et al. (2012) Serotonin and melatonin secretion and metabolism in patients with hepatic cirrhosis. Pol. Arch. Med. Wewn. 122: 392-397.
123. Messner M, Huether G, Lorf T, et al. (2001) Presence of melatonin in the human hepatobiliary-gastrointestinal tract. Life Sci. 69: 543–551.
124. Lee PPN, Shiu SYU, Chow PH, et al. (1995) Regional and diurnal studies on melatonin binding sites in the duck gastrointestinal tract. Biol. Signals 4: 212–224.
125. Chow PH, Lee PN, Poon AMS, et al. (1996) The gastrointestinal system: A site of melatonin paracrine action. In: Tang PL, Pang SF, Reiter RJ (eds.) Melatonin: A universal photoperiodic signal with diverse action. Frontiers of hormone research, Basel, Karger, 21: 123–132.
126. Quay WB, Ma YH (1976) Demonstration of gastro-intestinal hydroxyindole-O-methyltransferase. IRCS Med. Sci. 4: 563.
127. Stefulj J, Hörtner M, Ghosh M, et al. (2001) Gene expression of the key enzymes of melatonin synthesis in extrapineal tissues of the rat. J. Pineal Res. 30: 243–247.
128. Glaser S, Han Y, Francis H, et al. (2014) Melatonin regulation of biliary functions. Hepatobiliary Surg. Nutr. 3: 35-43. doi: 10.3978/j.issn.2304-3881.2013.10.04.
129. Chascsa D, Carey EJ, Lindor KD (2017) Old and new treatments for primary biliary 469 cholangitis. Liver Int. 37: 490-499. doi: 10.1111/liv.13294.
130. Lopez PM, Finana IT, De Agueda MC, et al. (2000) Protective effect of melatonin against oxidative stress induced by ligature of extra-hepatic biliary duct in rats: comparison with the effect of S-adenosyl-L-methionine. J. Pineal Res. 28: 143-149. https://doi.org/10.1034/j.1600-079X.2001.280303.x.
131. Renzi A, DeMorrow S, Onori P, et al. (2013) Modulation of the biliary expression of arylalkylamine N-acetyltransferase alters the autocrine proliferative responses of cholangiocytes in rats. Hepatology 57: 1130-1141. doi: 10.1002/hep.26105.
132. Han Y, Onori P, Meng F, et al. (2014) Prolonged exposure of cholestatic rats to complete dark inhibits biliary hyperplasia and liver fibrosis. Am. J. Physiol. Gastrointest. Liver Physiol. 307: G894–G904. doi:10.1152/ajpgi. 00288.2014.
133. McMillin M, DeMorrow S, Glaser S, et al. (2017) Melatonin inhibits hypothalamic gonadotropin-releasing hormone release and reduces biliary hyperplasia and fibrosis in cholestatic rats. Am. J. Physiol. Gastrointest. Liver Physiol. 313: G410-G418. https://doi.org/10.1152/ajpgi.00421.2016.
134. Kyritsi K, Meng F, Zhou T, et al. (2017) Knockdown of hepatic gonadotropin-releasing hormone by vivo- morpholino decreases liver fibrosis in multidrug resistance gene 2 knockout mice by down- regulation of mir-200b. Am. J. Pathol. 187: 1551-1565. doi: 10.1016/j.ajpath.2017.03.013.
135. Gibson P, Gill JH, Khanetal PA (2003) Cytochrome P450 1B1 (CYP1B1) is overexpressed in human colon adenocarcinomas relative to normal colon: implications for drug development. Mol. Cancer Ther. 2:527–534.
136. Kvetnoy IM, Ingel IE, Kvetnaia TV et al. (2002) Gastrointestinal melatonin: cellular identification and biological role. Neuro. Endocrinol. Lett. 23:121–132.
137. Reiter RJ, Tan DX, Mayo JC, et al. (2003) Neurally-mediated and neurally-independent beneficial actions of melatonin in the gastrointestinal tract. J. Physiol. Pharmacol. 54: 113–125.
138. Bubenik GA, Pang SF, Cockshutetal JR (2000) Circadian variation of portal, arterial and venous blood levels of melatonin in pigs and its relationship to food intake and sleep. J. Pineal Res. 28: 9-15. doi: 10.1034/j.1600-079x.2000.280102.x.
139. Lane EA, Noss HB (1985) Pharmacokinetics of melatonin in man: first pass hepatic metabolism. J. Clin. Endocrinol. Metab. 61: 1214-1216.
140. Facciolá G, Hidestrand M, vonBahr C, et al. (2001) Cytochrome P450 isoforms involved in melatonin metabolism in human liver microsomes. Eur. J. Clin. Pharmacol. 56: 881–888. doi: 10.1007/s002280000245.
141. Ma X, Idle JR, Krausz KW, et al. (2005) Metabolism of melatonin by human cytochromes P450. Drug Metab. Dispos. 33 (4): 489-494. doi: 10.1124/dmd.104.002410.
142. Steindl PE, Ferenci P, Marktl W (1997) Impaired hepatic catabolism of melatonin in cirrhosis. Ann. Intern. Med. 127: 494. https://doi.org/10.7326/0003-4819-127-6-199709150-00025.
143. Ardizzi A, Grugni G, Saglietti G, et al. (1998) Circadian rhythm of melatonin (aMT) in liver cirrhosis. Minerva Medica 89: 1–4.
144. Montagnese S, Middleton B, Mani AR, et al. (2010) On the origin and the consequences of circadian abnormalities in patients with cirrhosis. Am. J. Gastroenterol. 105: 1773-1781. doi: 10.1038/ajg.2010.86.
145. Celinski K, Konturek PC, Slomkaetal M (2009) Altered basal and postprandial plasma melatonin, gastrin, ghrelin, leptin and insulin in patients with liver cirrhosis and portal hypertension without and with oral administration of melatonin or tryptophan. J. Pineal Res. 46: 408– 414. doi: 10.1111/j.1600-079X.2009.00677.x.
146. Li M, Pi H, Yang Z, Reiter RJ, et al. (2016) Melatonin antagonizes cadmium-induced neurotoxicity by activating the transcription factor EB-dependent autophagy-lysosome machinery in mouse neuroblastoma cells. J. Pineal Res. 61: 353-69. doi: 10.1111/jpi.12353.
147. León J, Acuña-Castroviejo D, Escames G, et al. (2005) Melatonin mitigates mitochondrial malfunction. J. Pineal Res. 38: 1–9. doi: 10.1111/j.1600-079x.2004.00181.x.
148. Sener G, Sehirli AO, Ayanoglu-Dülger G (2003) Melatonin protects against mercury (II)-induced oxidative tissue damage in rats. Pharmacol. Toxicol. 93: 290-296.
149. Mishra S, Ghosh D, Dutta M, et al. (2013) Melatonin protects against lead-induced oxidative stress in stomach, duodenum and spleen of male Wistar rats. J. Pharm. Res. 1: 997-1004.
150. Konturek PC, Konturek SJ, Majka J, et al. (1997) Melatonin affords protection against gastric lesions induced by ischemia-reperfusion possibly due to its antioxidant and mucosal microcirculatory effects. Eur. J. Pharmacol. 322: 73–77. https://doi.org/10.1016/S0014-2999(97)00051-4.
151. Cabeza J, Alarcón-de-la-Lastra C, Jiménez D, et al. (2003) Melatonin modulates the effects of gastric injury in rats: role of prostaglandins and nitric oxide. Neurosignals 12: 71–77.doi: 10.1159/000071816.
152. Ozturk H, Oztürk H, Yagmur Y, et al. (2006) Effects of melatonin administration on intestinal adaptive response after massive bowel resection in rats. Dig. Dis. Sci. 51: 333–337. doi: 10.1007/s10620-006-3134-y.
153. Hardeland R, Tan DX, Reiter RJ (2009) Kynuramines, metabolites of melatonin and other indoles: the resurrection of an almost forgotten class of biogenic amines. J. Pineal Res. 47: 109–124. doi: 10.1111/j.1600-079x.2009.00701.x.
154. Gitto E, Pellegrino S, Gitto P, et al. (2009) Oxidative stress of the newborn in the pre-and postnatal period and the clinical utility of melatonin. J. Pineal Res. 44: 128–139. doi: 10.1111/j.1600-079x.2008.00649.x.
155. Martín M, Macías M, León J, et al. (2002) Melatonin increases the activity of the oxidative phosphorylation enzymes and the production of ATP in rat brain and liver mitochondria. Int. J. Biochem. Cell. Biol. 34: 348–357.
156. Acuña-Castroviejo D, Escames G, León J, et al. (2003) Mitochondrial regulation by melatonin and its metabolites. Adv. Exp. Med. Biol. 527: 549–557.
157. Bandyopadhyay D, Ghosh G, Bandyopadhyay A, et al. (2004) Melatonin protects against piroxicam-induced gastric ulceration. J. Pineal Res. 36: 195–203. https://doi.org/10.1111/j.1600-079X.2004.00118.x.
158. Jaworek J, Brzozowski T, Konturek SJ (2005) Melatonin as an organoprotector in the stomach and the pancreas. J. Pineal Res. 38: 73–83. doi: 10.1111/j.1600-079x.2004. 00179.x.
159. Ganguly K, Maity P, Reiter RJ, et al. (2005) Effect of melatonin on secreted and induced matrix metalloproteinase -9 and -2 activity during prevention of indomethacin-induced gastric ulcer. J. Pineal Res. 39: 307–315. doi: 10.1111/j.1600-079x.2005.00250.x.
160. Ganguly K, Kundu P, Banerjee A, et al. (2006) Hydrogen peroxide-mediated down regulation of matrixmetalloprotease-2 in indomethacin-induced acute gastric ulceration is blocked by melatonin and other antioxidants. Free Radic. Biol. Med. 41: 911–925. https://doi.org/10.1016/j.freeradbiomed.2006.04.022.
161. Konturek PC, Konturek SJ, Burnat G, et al. (2008) Dynamic physiological and molecular changes in gastric ulcer healing achieved by melatonin and its precursor L-tryptophan in rats. J. Pineal Res. 45: 180–190. doi: 10.1111/j.1600-079x.2008.00574.x.
162. Brzozowska I, Konturek PC, Brzozowski T, et al. (2002) Role of prostaglandins, nitric oxide, sensory nerves and gastrin in acceleration of ulcer healing by melatonin and its precursor, L-tryptophan. J. Pineal Res. 32: 149–162. https://doi.org/10.1034/j.1600-079x.2002.1o811.x.
163. Brzozowski T, Konturek PC, ZwirskaKorczala K, et al. (2005) Importance of the pineal gland, endogenous prostaglandins and sensory nerves in the gastroprotective actions of central and peripheral melatonin against stress-induced damage. J. Pineal Res. 39: 375–385. https://doi.org/10.1111/j.1600-079X.2005.00264.x.
164. Ricardo Rde S (2006) Regression of gastroesophageal reflux disease symptoms using dietary supplementation with melatonin, vitamins and aminoacids: comparison with omeprazole. J. Pineal Res. 41 (3): 195‐200. doi:10.1111/j.1600-079X.2006.00359.x.
165. Konturek PC, Konturek SJ, Brzozowski T (2006) Gastric cancer and Helicobacter pylori infection. J. Physiol. Pharmacol. 57 (Suppl 3): 51-65.
166. Bubenik GA, Ayles HL, Ball RO, et al. (1998) Relationship between melatonin levels in plasma and gastrointestinal tissues and the incidence and severity of gastric ulcers in pigs. J. Pineal Res. 24: 62–66. https://doi.org/10.1111/j.1600-079X.1998.tb00367.x.
167. Konturek SJ, Konturek PC, Brzozowska I, et al. (2007) Localization and biological activities of melatonin in intact and diseased gastrointestinal tract (GIT). J. Physiol. Pharmacol. 58 (3): 381-405.
168. Bandyopadhyay D, Bandyopadhyay A, Das PK, et al. (2002) Melatonin protects against gastric ulceration and increases the efficacy of ranitidine and omeprazole in reducing gastric damage. J. Pineal Res. 33: 1-7. https://doi.org/10.1034/j.1600-079X.2002. 01107.x.
169. Bandyopadhyay D, Chattopadhyay A (2006) Reactive oxygen species-induced gastric ulceration: protection by melatonin. Curr. Med. Chem. 13: 1187–1202. doi: 10.2174/ 092986706776360842.
170. Witt-Enderby PA, Radio NM, Doctor JS, et al. (2006) Therapeutic treatments potentially mediated by melatonin receptors: potential clinical uses in the prevention of osteoporosis, cancer and as an adjuvant therapy. J. Pineal Res. 41: 297–305. doi: 10.1111/j.1600-079x.2006.00369.x.
171. Lopez-Burillo S, Tan DX, Rodriguez-Gallego V, et al. (2003) Melatonin and its derivatives cyclic 3-hydroxymelatonin, N1-acetyl-N2-formyl-5- methoxykynuramine, and 6-hydroxymelatonin reduced oxidative damage induced by Fenton reagents. J. Pineal Res. 34: 237–256. doi: 10.1034/j.1600-079x.2003.00025.x.
172. Nosál'ová V, Zeman M, Černá S, et al. (2007) Protective effect of melatonin in acetic acid induced colitis in rats. J. Pineal Res. 42: 364–370. doi: 10.1111/j.1600-079X.2007.00428.x.
173. Srinivasan V, Lauterbach EC, Ho KY, et al. (2012) Melatonin in antinociception: Its therapeutic applications. Curr. Neuropharmacol. 10: 167–178. doi: 10.2174/157015912800604489.
174. Cuzzocrea S, Reiter JR (2002) Pharmacological action of melatonin in acute and chronic inflammation. Curr. Top. Med. Chem. 2:153–165.
175. Carrillo-Vico A, Lardone PJ, Alvarez-Sánchez N, et al. (2013) Melatonin: buffering the immune system. Int. J. Mol. Sci. 14: 8638–8683. doi: 10.3390/ijms14048638.
176. Maldonado MD, Reiter RJ, Pérez‐San‐Gregorio MA (2016) Melatonin as a potential therapeutic agent in psychiatric illness. J. Pineal Res. 24: 391-400. https://doi.org/ 10.1002/ hup.1032.
177. Carrasco C, Marchena AM, Holguín-Arévalo MS, et al. (2013) Anti-inflammatory effects of melatonin in a rat model of caerulein-induced acute pancreatitis. Cell. Biochem. Funct. 31 (7): 585-590. doi: 10.1002/cbf.2942.
178. Carrasco C, Rodriguez AB, Pariente JA (2014) Effects of melatonin on the oxidative damage and pancreatic antioxidant defenses in cerulein-induced acute pancreatitis in rats. Hepatobiliary Pancreat. Dis. Int. 13 (4): 442-446. doi: 10.1016/s1499-3872(14)60271-x.
179. Han Y, DeMorrow S, Invernizzi P, et al. (2011) Melatonin exerts by an autocrine loop antiproliferative effects in cholangiocarcinoma: its synthesis is reduced favoring cholangiocarcinoma growth. Am. J. Physiol. Gastrointest. Liver Physiol. 301: G623-G633. doi: 10.1152/ajpgi.00118.2011.
180. Lesage G, Glaser S, Ueno Y, et al. (2001) Regression of cholangiocyte proliferation after cessation of ANIT feeding is coupled with increased apoptosis. Am. J. Physiol. Gastrointest. Liver Physiol. 281: G182-G190. doi: 10.1152/ajpgi.2001.281.1.G182.
181. Ohta Y, Kongo-Nishimura M, Imai Y, et al. (2006) alpha- Tocopherol protects against alpha-naphthylisothiocyanate-induced hepatotoxicity in rats less effectively than melatonin. Chem. Biol. Interact. 161: 115-124. https://doi.org/10.1016/j.cbi.2006.03.006.
182. Laothong U, Pinlaor P, Boonsiri P, et al. (2013) Melatonin inhibits cholangiocarcinoma and reduces liver injury in Opisthorchis viverrini-infected and N-nitrosodimethylamine-treated hamsters. J. Pineal Res. 55: 257-266. doi: 10.1111/jpi.12068.
183. Sumova A, Vanecek J (1997) Melatonin inhibits GnRH-induced increase of cFOS immunoreactivity in neonatal rat pituitary. J. Neuroendocrinol. 9: 135–139. https://doi.org/10.1046/j.1365-2826.1997.d01-1076.x.
184. Vanecek J (1999) Inhibitory effect of melatonin on GnRH-induced LH release. Rev. Reprod. 4: 67-72. doi:10.1530/ror.0.0040067.
185. Han Y, Meng F, Venter J, et al. (2016) miR-34a-dependent 535 overexpression of Per1 decreases cholangiocarcinoma growth. J. Hepatol. 64: 1295-1304. doi: 10.1016/j.jhep.2016.02.024.
186. Blask DE, Dauchy RT, Sauer LA, et al. (2004) Melatonin uptake and growth prevention in rat hepatoma 7288CTC in response to dietary melatonin: melatonin receptor-mediated inhibition of tumor linoleic acid metabolism to the growth signaling molecule 13-hydroxyoctadecadienoic acid and the potential role of phytomelatonin. Carcinogenesis 25: 951-960. doi: 10.1093/carcin/bgh090.
187. Lissoni P, Barni S, Tancini G, et al. (1993) Immunotherapy with subcutaneous low-dose interleukin-2 and the pineal indole melatonin as a new effective therapy in advanced cancers of the digestive tract. Br. J. Cancer 67: 1404-1407. doi: 10.1038/bjc.1993.260.
188. Yan JJ, Shen F, Wang K, et al. (2002) Patients with advanced primary hepatocellular carcinoma treated by melatonin and transcatheter arterial chemoembolization: a prospective study. Hepatobiliary Pancreat. Dis. Int. 1: 183-186.
189. Tahan V, Ozaras R, Canbakan B, et al. (2004) Melatonin reduces dimethylnitrosamine-induced liver fibrosis in rats. J. Pineal Res. 37: 78-84. doi: 10.1111/j.1600-079X.2004.00137.x.
190. Cruz A, Padillo FJ, Torres E, et al. (2005) Melatonin prevents experimental liver cirrhosis induced by thioacetamide in rats. J. Pineal Res. 39: 143-150. https://doi.org/10.1111/j.1600-079X.2005.00227.x.
191. Koc M, Taysi S, Buyukokuroglu ME (2003) Melatonin protects rat liver against irradiation-induced oxidative injury. J. Radiat. Res. 44 (3): 211-215.
192. Sewerynek E, Reiter RJ, Melchiorri D, et al. (1996) Oxidative damage in the liver induced by ischemia-reperfusion: protection by melatonin. Hepato-Gastroenterology 43 (10): 898-905.
193. Vairetti M, Ferrigno A, Bertoneetal R (2005) Exogenous melatonin enhances bile flow and ATP levels after cold storage and reperfusion in rat liver: implications for liver transplantation. J. Pineal Res. 38 (4): 223-230. doi: 10.1111/j.1600-079X.2004.00193.x.
194. Zaoualí MA, Reiter RJ, Padrissa-Altés S, et al. (2011) Melatonin protects steatotic and nonsteatotic liver grafts against cold ischemia and reperfusion injury. J. Pineal Res. 50 (2): 213–221. doi: 10.1111/j.1600-079X.2010.00831.x.
195. Daniels WM, Reiter RJ, Melchiorri D, et al. (1995) Melatonin counteracts lipid peroxidation induced by carbon tetrachloride but does not restore glucose-6 phosphatase activity. J. Pineal Res.19 (1): 1-6. doi: 10.1111/j.1600-079x.1995.tb00164.x.
196. Sahna E, Parlakpinar H, Vardi N, et al. (2004) Efficacy of melatonin as protectant against oxidative stress and structural changes in liver tissue in pinealectomized rats. Acta Histochemica. 106 (5): 331-336. https://doi.org/10.1016/j.acthis.2004.07.006.
197. Reiter RJ, Paredes SD, Manchester LC, et al. (2009) Reducing oxidative/nitrosative stress: a newly-discovered genre for melatonin. Crit. Rev. Biochem. 44 (4): 175-200. doi: 10.1080/10409230903044914.
198. Mathes AM (2010) Hepatoprotective actions of melatonin: possible mediation by melatonin receptors. World J. Gastroenterol. 16 (48): 6087-6097. doi: 10.3748/wjg.v16. i48.6087.
199. Hong RT, Xu JM, Mei Q (2009) Melatonin ameliorates experimental hepatic fibrosis induced by carbon tetrachloride in rats. World J. Gastroenterol. 15 (12): 1452-1458. doi: 10.3748/wjg.15.1452.
200. Rosa DP, Bona S, Simonetto D, et al. (2010) Melatonin protects the liver and erythrocytes against oxidative stress in cirrhotic rats. Arq. Gastroenterol. 47: 72-78.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.