Melatonin as a potential therapeutic molecule against myocardial damage caused by high fat diet (HFD)
Protective role of melatonin against high fat diet-induced cardiac injury
Abstract
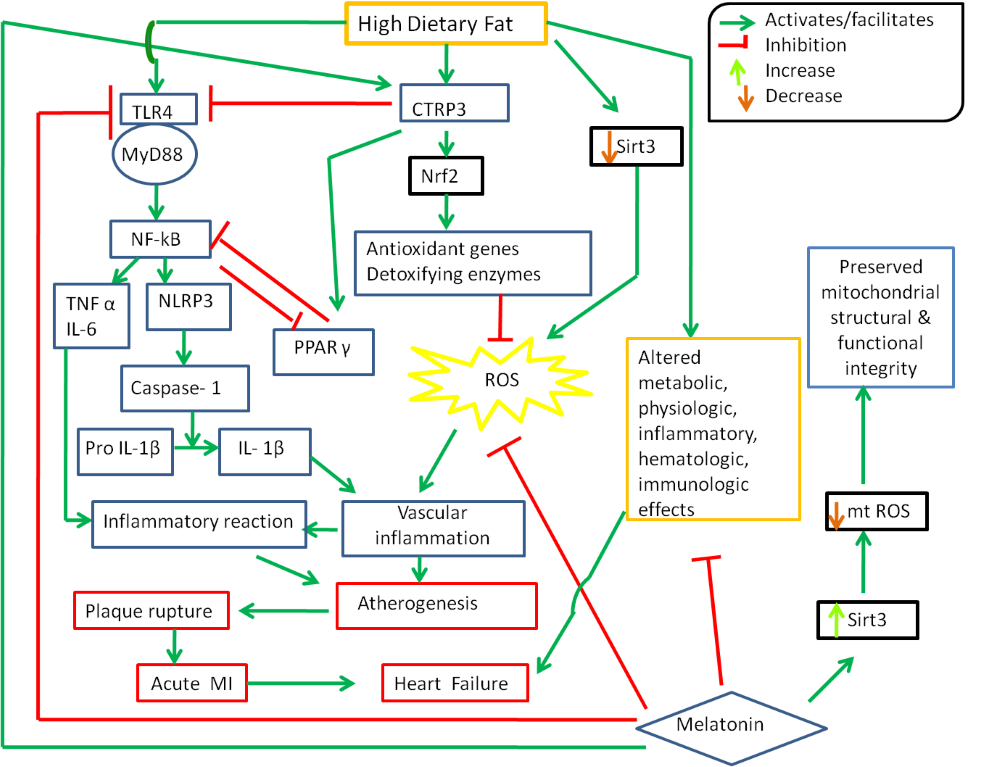
High fat diet (HFD) has been implicated as an independent risk factor for cardiovascular diseases since the second half of the last century. The HFD causes various pathogeneses and progressions of cardiovascular diseases. The oxidative stress and pro-inflammatory reactions induced by the HFD are probably the major risk factors of myocardial damage. In this review we highlight the roles of different dietary fats on cardiovascular diseases and the protective effects of melatonin as a potent antioxidant and anti-inflammation molecule on the pathology induced by HFD. The focus will be given to the molecular mechanisms. The protective effects of melatonin on HFD induced myocardial damage are mediated by multiple pathways. These include that melatonin suppresses the oxidative stress, preserves the normal fat and glucose metabolisms and reduces the pro-inflammatory reactions. Melatonin downregulates the expressions of pro-inflammatory genes of TLR4, NF-κB and NLRP3-Caspase1 but upregulates the expressions of anti-inflammatory genes of Sirt3, CTRP3 and RISK. All of these render melatonin as a powerful protector against cardiovascular diseases caused by the HFD. This review suggests that melatonin can be used as a therapeutic agent in this specific condition.
References
2. WHO (2003) Diet, Nutrition and the prevention of chronic diseases. WHO Technical Report series 916. Pp. 1-148.
3. Popkin BM, Adair LS, Ng SW (2012) Now and then: the global nutrition transition: the pandemic of obesity in developing countries. Nutr. Rev. 70 (1): 3–21. doi:10.1111/j.1753-4887.2011.00456.x.
4. Ferretti F, Mariani M (2019) Sugar-sweetened beverage affordability and the prevalence of overweight and obesity in a cross section of countries. Global Health 15: 30. https://doi.org/10.1186/s12992-019-0474-x.
5. Ballal K, Wilson CR, Harmancey R, Taegtmeyer H (2010) Obesogenic high fat western diet induces oxidative stress and apoptosis in rat heart. Mol. Cell Biochem.344: 221–230. doi 10.1007/s11010-010-0546-y.
6. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan R (2002) Obesity and the risk of heart failure. N. Engl. J. Med. 347: 305–313. doi: 10.1056/NEJMoa020245.
7. Asgharpour A, Cazanave SC, Pacana T, Seneshaw M, Vincent R, Banini BA, Kumar DP, Daita K, Min HK, Mirshahi F, Bedossa P, Sun X, Hoshida Y, Koduru SV, Contaifer Jr. D, Warncke UO, Wijesinghe DS, Sanyal AJ (2016) A diet-induced animal model of non-alcoholic fatty liver disease and hepatocellular cancer. J. Hepatol. 65: 579–588. doi: 10.1016/j.jhep.2016.05.005.
8. Kuller LH (1997) Dietary fat and chronic diseases: epidemiologic overview. J. Am. Diet. Assoc.97 (7 Suppl): S9-15.
9. Weisburger JH (1997) Dietary fat and risk of chronic diseases: mechanistic insights from experimental studies. J. Am. Diet. Assoc.97 (7 Suppl): S16-23.
10. Wang M, Ma LJ, Yang Y, Xiao Z, WanJB (2018) n-3 Polyunsaturated fatty acids for the management of alcoholic liver disease: A critical review. Crit. Rev. Food Sci. Nutr. 22:1-14. doi: 10.1080/10408398.2018.1544542.
11. Svendsen K, Arnesen E, Retterstol K (2017) Saturat¬ed fat – a never ending story? Food Nutr. Res. 61 (1): 1377572. doi: 10.1080/16546628.2017.1377572.
12. Hooper L, Martin N, Abdelhamid A, Davey Smith G (2015) Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst. Rev.10 (6): CD011737. doi: 10.1002/14651858.CD011737.
13. Li Y, Hruby A, Bernstein AM, Ley SH (2015) Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J. Am. Coll. Cardiol. 66 (14): 1538-1548. doi: 10.1016/j.jacc.2015.07.055.
14. Mozaffarian D, Micha R, Wallace S (2010) Effects on coronary heart disease of increasing polyun¬saturated fat in place of saturated fat: a system¬atic review and meta-analysis of randomized controlled trials. PLoS Med. 7 (3): e1000252. doi: 10.1371/journal.pmed.1000252.
15. Lian Y, Xia X, Zhao H, Zhu Y (2017) The potential of chrysophanol in protecting against high fat-induced cardiac injury through Nrf2-regulated anti-inflammation, anti-oxidant and anti-fibrosis in Nrf2 knockout mice. Biomed. Pharmacother. 93: 1175-1189. doi: 10.1016/j.biopha.2017.05.148.
16. Xu Z, Kong XQ (2017) Bixin ameliorates high fat diet-induced cardiac injury in mice through inflammation and oxidative stress suppression. Biomed. Pharmacother. 89: 991-1004. doi: 10.1016/j.biopha.2017.02.052.
17. Vargas-Robles H, Rios A, Arellano-Mendoza M, Escalante BA, Schnoor M (2015) Antioxidative diet supplementation reverses high-fat diet-induced increases of cardiovascular risk factors in mice. Oxid. Med. Cell Longev. 2015: 467-471. doi: 10.1155/2015/467471.
18. Reiter RJ, Tan DX, Osuna C, Gitto E (2000) Actions of melatonin in the reduction of oxidative stress. A review. J. Biomed. Sci. 7 (6): 444-458.doi: 10.1159/000025480.
19. Tan DX, Manchester LC, Reiter RJ, Qi W, Kim SJ, El-Sokkary GH (1998) Ischemia/reperfusion-induced arrhythmias in the isolated rat heart: prevention by melatonin. J. Pineal Res. 25 (3): 184-191.https://doi.org/10.1111/j.1600-079X. 1998.tb00558.x.
20. Mukherjee D, Roy SG, Bandyopadhyay A, Chattopadhyay A, Basu A, Mitra E, Ghosh AK, Reiter RJ, Bandyopadhyay D (2010) Melatonin protects against isoproterenol-induced myocardial injury in the rat: antioxidative mechanisms. J. Pineal Res. 48 (3): 251-262. doi: 10.1111/j.1600-079X.2010.00749.x.
21. Van Gaal LF, Mertens IL, De Block CE (2006) Mechanisms linking obesity with cardiovascular disease. Nature 444 (7121): 875–880. doi: 10.1038/nature05487.
22. Auberval N, Dal S, Bietiger W, Pinget M, Jeandidier N, Maillard-Pedracini E, Schini-Kerth V, Sigrist S (2014) Metabolic and oxidative stress markers in Wistar rats after 2 months on a high-fat diet. Diabetol. Metab. Syndr. 6: 130. doi: 10.1186/1758-5996-6-130.
23. DiNicolantonio JJ, Lucan SC, O’Keefe JH (2016) The evidence for saturated fat and for sugar related to coronary heart disease. Prog. Cardiovasc. Dis. 58 (5) :464-472. https://doi.org/10.1016/j.pcad.2015.11.006.
24. Sorof J, Daniels S (2002) Obesity hypertension in children: a problem of epidemic proportions. Hypertension 40 (4): 441-447. doi: 10.1161/01.hyp.0000032940.33466.12.
25. Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM (2012) National, regional, and global trends in adult overweight and obesity prevalences. Popul. Health Metr.10 (1): 22. doi: 10.1186/1478-7954-10-22.
26. Picchi MG1, Mattos AM, Barbosa MR, Duarte CP, Gandini Mde A, Portari GV, Jordão AA (2011) A high-fat diet as a model of fatty liver disease in rats. Acta Cirúrgica Brasileira. 26 (Suppl. 2): 25-30.
27. Arita S, Kinoshita Y, Ushida K, Enomoto A, Inagaki-Ohara K (2016) High fat diet feeding promotes stemness and precancerous changes in murine gastric mucosa mediated by leptin receptor signaling pathway. Arch Biochem. Biophys. 610: 16–24. doi: 10.1016/j.abb.2016.09.015.
28. Hu J, La Vecchia C, Negri E, de Groh M, Morrison H, Mery L (2015) Macronutrient intake and stomach cancer. Cancer Causes Control 26 (6): 839-847. doi: 10.1007/s10552-015-0557-9.
29. Wolfson B, Zhang Y, Gernapudi R, Duru N, Yao Y, Lo PK (2017) A high fat diet promotes mammary gland myofibroblast differentiation through microRNA 140 downregulation. Mol. Cell. Biol. 37 (4): e00461-16. doi: 10.1128/MCB.00461-16.
30. Wolf MJ, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, Ringelhan M, Simonavicius N, Egger M, Wohlleber D, Lorentzen A, Einer C, Schulz S, Clavel T, Protzer U, Thiele C, Zischka H, Moch H, Tschöp M, Tumanov AV, Haller D, Unger K, Karin M, Kopf M, Knolle P, Weber A, Heikenwalder M (2014) Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 26 (4): 549-564. doi: 10.1016/j.ccell.2014.09.003.
31. Delgado TC, Pinheiro D, Caldeira M, Castro MM, Geraldes CF, López-Larrubia P, Cerdán S, Jones JG (2009) Sources of hepatic triglyceride accumulation during high-fat feeding in the healthy rat. NMR Biomed. 22 (3): 310-307. doi: 10.1002/nbm.1327.
32. Alberdi G, Rodríguez VM, Macarulla MT, Miranda J, Churruca I, Portillo MP (2013) Hepatic lipid metabolic pathways modified by resveratrol in rats fed an obesogenic diet. Nutrition 29 (3): 562-567. doi: 10.1016/j.nut.2012.09.011.
33. Milagro FI, Campión J, Martínez JA (2006) Weight gain induced by high-fat feeding involves increased liver oxidative stress. Obesity (Silver Spring) 14 (7): 1118-1123.doi: 10.1038/oby.2006.128.
34. Jaskiewicz K, Rzepko R, Sledzinski Z (2008) Fibrogenesis in fatty liver associated with obesity and diabetes mellitus type 2. Dig. Dis. Sci. 53 (3): 785-788. doi: 10.1007/s10620-007-9942-x.
35. Leclercq IA (2007) Pathogenesis of steatohepatitis: Insights from the study of animal models. Acta Gastroenterol. Belg. 70 (1): 25-31.
36. Zou Y, Li J, Lu C, Wang J, Ge J, Huang Y (2006) High-fat emulsion-induced rat model of nonalcoholic steatohepatitis. Life Sci. 79: 1100-1107. doi: 10.1016/j.lfs.2006.03.021.
37. Bellanti F, Villani R, Facciorusso A,Vendemiale G, Serviddio G (2017) Lipid oxidation products in the Pathogenesis of non-alcoholic Steatohepatitis. Free Radic. Biol. Med. 111: 173-185. doi: 10.1016/j.freeradbiomed.2017.01.023.
38. Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, Amma LI, Avezum A, Chifamba J, Diaz R, Khatib R, Lear S, Lopez-Jaramillo P, Liu X, Gupta R, Mohammadifard N, Gao N, Oguz A, Ramli AS, Seron P, Sun Y, Szuba A, Tsolekile L, Wielgosz A, Yusuf R, Hussein Yusufali A, Teo KK, Rangarajan S, Dagenais G, Bangdiwala SI, Islam S, Anand SS, Yusuf S (2017) Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 390 (10107): 2050-2062. doi:10.1016/S0140-6736(17)32252-3.
39. Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, Hegele RA, Krauss RM, Raal FJ, Schunkert H, Watts GF, Borén J, Fazio S, Horton JD, Masana L, Nicholls SJ, Nordestgaard BG, van de Sluis B, Taskinen MR, Tokgözoglu L, Landmesser U, Laufs U, Wiklund O, Stock JK, Chapman MJ, Catapano AL (2017) Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38 (32): 2459-2472. doi: 10.1093/eurheartj/ehx144.
40. Micha R, Mozaffarian D (2010) Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids 45 (10): 893-905. doi:10.1007/s11745-010-3393-4 20354806.
41. Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG, Stone NJ, Van Horn LV (2017) Dietary fats and cardiovascular disease: a presidential advisory from the american heart association. Circulation 136 (3): 1-23. doi: 10.1161/CIR.0000000000000510 28620111.
42. Cano P, Cardinali DP, Ríos‐Lugo M J, Fernández‐Mateos MP, Toso CF, Esquifino AI (2009) Effect of a high‐fat diet on 24‐hour pattern of circulating adipocytokines in rats. Obesity 17 (10): 1866-1871. doi:10.1038/oby.2009.200.
43. Stemmer K, Perez-Tilve D, Ananthakrishnan G, Bort A, Seeley RJ, Tschöp MH, Dietrich DR, Pfluger PT (2012) High-fat-diet-induced obesity causes an inflammatory and tumor-promoting microenvironment in the rat kidney. Dis. Model Mech. 5: 627-635. doi:10.1242/dmm.009407.
44. Denver P, Gault VA, McClean PL (2018) Sustained high fat diet modulates inflammation, insulin signalling and cognition in mice and a modified xenin peptide ameliorates neuropathology in a chronic high fat model. Diabetes Obes. Metab. 20 (5): 1166-1175. https://doi.org/10.1111/dom.13210.
45. Murray AJ, Knight NS, Cochlin LE, McAleese S, Deacon RMJ, Rawlins JNP, Clarke K (2009) Deterioration of physical performance and cognitive function in rats with short-term high-fat feeding. FASEB J. 23 (12): 4353-4360. doi: 10.1096/fj.09-139691.
46. Pendergast JS, Branecky KL, Yang W, Ellacott KLJ, Niswender KD, Yamazaki S (2013) High-fat diet acutely affects circadian organization and eating behaviour.Eur. J. Neurosci.37 (8): 1350–1356. doi:10.1111/ejn.12133.
47. Hansen PA, Han DH, Marshall BA, Nolte LA, Chen MM, Mueckler M, Holloszy JO (1998) A high fat diet impairs stimulation of glucose transport in muscle. Functional evaluation of potential mechanisms. J. Biol. Chem. 273 (40): 26157-26163. doi: 10.1074/jbc.273.40.26157.
48. Kohsaka A, Laposky AD, Ramsey KM, Estrada C, Joshu C, Kobayashi Y, Turek FW, Bass J (2007) High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell Metab. 6 (5): 414-421. doi: 10.1016/j.cmet.2007.09.006.
49. Dobbins RL, Szczepaniak LS, Bentley B (2001) Prolonged inhibition of muscle carnitine palmitoyltransferase-1 promotes intramyocellular lipid accumulation and insulin resistance in rats. Diabetes 50: 123–130.
50. Schaffer JE (2003) Lipotoxicity: when tissues overeat. Curr. Opin. Lipidol. 14: 281–287. doi: 10.1097/01.mol.0000073508.41685.7f.
51. Lavie CJ, Milani RV, Ventura HO (2009) Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J. Am. Coll. Cardiol. 53 (21): 1925–1932.
52. Jeckel KM, Miller KE, Chicco AJ, Chapman PL, Mulligan CM, Falcone PH, Miller ML, Pagliassotti MJ, Frye MA (2011) The role of dietary fatty acids in predicting myocardial structure in fat-fed rats. Lipids Health Dis. 10: 92. doi: 10.1186/1476-511X-10-92.
53. Ebong IA, Goff Jr DC, Rodriguez CJ, Chen H, Bertoni AG (2014) Mechanisms of heart failure in obesity. Obes. Res. Clin. Pract. 8 (6): 540–548. doi: 10.1016/j.orcp.2013.12.005.
54. Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC (2006) Trans fatty acids and cardiovascular disease. N. Engl. J. Med. 354 (15): 1601-1613. doi: 10.1056/NEJMra054035.
55. Stanley WC, Dabkowski ER, Ribeiro Jr. RF, O'Connell KA (2012) Dietary fat and heart failure: moving from lipotoxicity to lipoprotection. Circ. Res. 110 (5): 764-776. doi: 10.1161/CIRCRESAHA.111.253104.
56. Jakobsen MU, O'Reilly EJ, Heitmann BL, Pereira MA, Bälter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A (2009) Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am. J. Clin. Nutr. 89 (5): 1425-1432. doi: 10.3945/ajcn.2008.27124.
57. Nettleton JA, Brouwer IA, Geleijnse JM, Hornstra G (2017) Saturated fat consumption and risk of coronary heart disease and ischemic stroke: a science update. Ann. Nutr. Metab. 70 (1): 26-33. doi: 10.1159/000455681.
58. Rizos EC, Ntzani EE, Bika E, Kostapanos MS, Elisaf MS (2012) Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events a systematic review and meta-analysis. JAMA. 308 (10): 1024-1033. doi: 10.1001/2012.jama.11374.
59. Helnaes A, Kyro C, Andersen I, Lacoppidan S, Overvad K, Christensen J, Tjonneland A, Olsen A (2016) Intake of whole grains is associated with lower risk of myocardial infarction: the Danish Diet, Cancer and Health Cohort. Am. J. Clin. Nutr. 103 (4): 999-1007. doi: 10.3945/ajcn.115.124271.
60. Keys A, Menotti A, Aravanis C, Blackburn H, Djordevic BS, Buzina R, Dontas AS, Fidanza F, Karvonen MJ, Kimura N, Mohacek I, Nedeljkovic IS, Puddu V, Punsar S, Taylor HL, Conti S, Kromhout D, Toshima H (1984) The seven countries study: 2,289 deaths in 15 years. Prev. Med. 13:141-154.
61. Balk EM, Lichtenstein AH, Chunga M, Kupelnick B, Chewa P, Laua J (2006) Effects of omega-3 fatty acids on serum markers of cardiovascular disease risk: A systematic review. Atherosclerosis 189: 19–30.
62. Parthasarathy S, Litvinov D, Selvarajan K, Garelnabi M (2008) Lipid peroxidation and decomposition – conflicting roles in plaque vulnerability and stability. Biochim. Biophys. Acta 1781: 221-231. doi:10.1016/j.bbalip.2008.03.002.
63. DiNicolantonio JJ, O’Keefe JH (2018) Omega-6 vegetable oils as a driver of coronary heart disease: the oxidized linoleic acid hypothesis. Open Heart 5 (2): e000898. http://dx.doi.org/10.1136/openhrt-2018-000898.
64. Farvid MS, Ding M, Pan A, Sun Q, Chiuve SE, Steffen LM, Willett WC, Hu FB (2014) Di¬etary linoleic acid and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Circulation 130 (18): 1568–1578. doi: 10.1161/CIRCULATIONAHA.114.010236.
65. Wu JH, Lemaitre RN, King IB, Song X, Psaty BM, Siscovick DS, Mozaffarian D (2014) Circulating omega-6 polyunsaturated fatty acids and total and cause-specific mortality: the cardiovascular health study. Circulation 130 (15): 1245-1253. doi: 10.1161/CIRCULATIONAHA.114.011590.
66. Raher MJ, Thibault HB, Buys ES, Kuruppu D, Shimizu N, Brownell AL, Blake SL, Rieusset J, Kaneki M, Derumeaux G, Picard MH, Bloch KD, Scherrer-Crosbie M (2008) A short duration of high-fat diet induces insulin resistance and predisposes to adverse left ventricular remodeling after pressure overload. Am. J. Physiol. Heart Circ. Physiol. 295 (6): H2495–H2502. doi: 10.1152/ajpheart.00139.2008.
67. Ouwens DM, Boer C, Fodor M, de Galan P, Heine RJ, Maassen JA, Diamant M (2005) Cardiac dysfunction induced by high-fat diet is associated with altered myocardial insulin signalling in rats. Diabetologia 48 (6): 1229-1237. doi: 10.1007/s00125-005-1755-x.
68. Preis SR, Pencina MJ, Hwang SJ, D’Agostino Sr RB, Savage PJ, Levy D, Fox CS (2009) Trends in cardiovascular disease risk factors in individuals with and without diabetes in the framingham heart study. Circulation 120 (3): 212–220. doi: 10.1161/CIRCULATIONAHA.108.846519.
69. Maulucci G, Daniel B, Cohen O, Avrahami Y, Sasson S (2016) Hormetic and regulatory effects of lipid peroxidation mediators in pancreatic beta cells. Mol. Asp. Med. 49: 49–77.doi: 10.1016/j.mam.2016.03.001.
70. Mangge H, Becker K, Fuchs D, Gostner JM (2014) Antioxidants, inflammation and cardiovascular disease. World J. Cardiol. 6 (6): 462-477. doi: 10.4330/wjc.v6.i6.462.
71. Pacher P, Beckman JS, Liaudet L (2007) Nitric oxide and peroxynitrite in health and disease. Physiol. Rev. 87: 315-424. doi: 10.1152/physrev.00029.2006.
72. Griendling KK, Sorescu D, Lassegue B, Ushio-Fukai M (2000) Modulation of protein kinase activity and gene expression by reactive oxygen species and their role in vascular physiology and pathophysiology. Arterioscler. Thromb. Vasc. Biol. 20: 2175-2183. doi:n10.1161/01.ATV.20.10.2175.
73. Litvinova L, Atochin DN, Fattakhov N, Vasilenko M, Zatolokin P, Kirienkova E (2015) Nitric oxide and mitochondria in metabolic syndrome. Front. Physiol. 6: 1-10. doi: 10.3389/fphys.2015.00020.
74. Ghosh A, Bose G, Dey T, Pal PK, Mishra S, Ghosh AK, Chattopadhyay A, Bandyopadhyay D (2019) Melatonin protects against cardiac damage induced by a combination of high fat diet and isoproterenol exacerbated oxidative stress in male Wistar rats. Melatonin Res.2 (1):9-31. doi: 10.32794/mr11250009.
75. Charradi K, Elkahoui S, Limam F, Aouani E (2013) High-fat diet induced an oxidative stress in white adipose tissue and disturbed plasma transition metals in rat: prevention by grape seed and skin extract. J. Physiol. Sci. 63: 445–455. doi: 10.1007/s12576-013-0283-6.
76. Bose G, Ghosh A, Mishra S, Dey T, Bandyopadhyay D (2017) High fat diet induced myocardial injury: a time response study. J. Pharm. Res. 11 (6):629-638.
77. Matsuzawa-Nagata N, Takamura T, Ando H, Nakamura S, Kurita S, Misu H, Ota T, Yokoyama M, Honda M, Miyamoto K, Kaneko S (2008) Increased oxidative stress precedes the onset of high-fat diet–induced insulin resistance and obesity. Metab. Clin. Experim. 57 (8): 1071-1077. doi: 10.1016/j.metabol.2008.03.010.
78. Chen YR, Zweier JL (2014) Cardiac mitochondria and reactive oxygen species generation. Circ. Res. Circ. Res. 114 (3): 524-537. doi: 10.1161/CIRCRESAHA.114.300559.
79. Walczewska A, Dziedzic B, Stepien T, Swiatek E, Nowak D (2010). Effect of dietary fats on oxidative-antioxidative status of blood in rats. J. Clin. Biochem. Nutr. 47 (1):18–26.doi:10.3164/jcbn.09-116.
80. Santos SHS, Andradec JMO, Fernandes LR, Sinisterrae RDM, Sousa FB, Feltenberger JD, Alvarez-Leiteb JI, Santos RAS (2013) Oral Angiotensin-(1–7) prevented obesity and hepatic inflammation byinhibition of resistin/TLR4/MAPK/NF-κB in rats fed with high-fat diet. Peptides 46: 47–52. doi: 10.1016/j.peptides.2013.05.010.
81. Kim KA, Gu W, Lee IA, Joh EH, Kim DH (2012) High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the tlr4signaling pathway. PLoS One 7 (10): e47713. doi:10.1371/journal.pone.0047713.
82. Zeng H, Vaka VR, He X, Booz GW, Chen JX (2015) High-fat diet induces cardiac remodelling and dysfunction:assessment of the role played by SIRT3 loss. J. Cell. Mol. Med. 19 (8): 1847-1856. doi: 10.1111/jcmm.12556.
83. Winklhofer-Roob BM, Faustmann G, Roob JM (2017) Low-density lipoprotein oxidation biomarkers in human health and disease and effects of bioactive compounds. Free Radic. Biol. Med. 111: 38-86. doi: 10.1016/j.freeradbiomed.2017.04.345.
84. Gregor MF, Hotamisligil GS (2011) Inflammatory Mechanisms in Obesity. Annu. Rev. Immunol. 29 (1): 415-445. https://doi.org/10.1146/annurev-immunol-031210-101322.
85. Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, Esquivel-Soto J, Morales-González A, Esquivel-Chirino C, Durante-Montiel I, Sánchez-Rivera G, Valadez-Vega C, Morales-González JA (2011) Inflammation, Oxidative Stress, and Obesity. Int. J. Mol. Sci.12 (5): 3117-3132. https://doi.org/10.3390/ijms12053117.
86. Saltiel AR, Olefsky JM (2017) Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Invest. 127 (1): 1-4. https://doi.org/10.1172/JCI92035.
87. Hsueh WA, Bruemmer D (2004) Peroxisome proliferator-activated receptor γ: implications for cardiovascular disease. Hypertension 43 (2): 297–305. https://doi.org/10.1161/01.HYP.0000113626.76571.5b.
88. Brock TG, McNish RW, Peters-Golden M (1999) Arachidonic acid is preferentially metabolized by cyclooxygenase-2 to prostacyclin and prostaglandin E2. J. Biol. Chem. 274 (11): 660–666.doi: 10.1074/jbc.274.17.11660.
89. Sonnweber T, Pizzini A, Nairz M, Weiss G, Tancevski I (2018) Arachidonic Acid Metabolites in Cardiovascular and Metabolic Diseases. Int. J. Mol. Sci. 19 (11): 3285 https://doi.org/10.3390/ijms19113285.
90. Cooper-DeHoff RM (2007) Metabolic syndrome and cardiovascular disease: challenges and opportunities. Clin. Cardiol. 30 (12): 593–597. doi: 10.1002/clc.7.
91. Ríos-Lugo MJ, Cano P, Jiménez-Ortega V, Fernández-Mateos MP, Scacchi PA, Cardinali DP, Esquifino AI. Melatonin effect on plasma adiponectin, leptin, insulin, glucose, triglycerides and cholesterol in normal and high fat-fed rats. J. Pineal Res. 49 (4): 342-348. doi: 10.1111/j.1600-079X.2010.00798.x.
92. Ghada M. Abou Fard, Nermin M. Madi, and Mervat H. El-Saka (2013) Effect of melatonin on obesity and lipid profile in high fat–fed rats. Am. Sci. 9 (10): 61-67. http://www.americanscience.org.
93. Agil A, Navarro-Alarcón M, Ruiz R, Abuhamadah S, El-Mir MY, Vázquez GF (2011) Beneficial effects of melatonin on obesity and lipid profile in young Zucker diabetic fatty rats. J. Pineal Res. 50 (2): 207-212. doi: 10.1111/j.1600-079X.2010.00830.x.
94. Fernández-Vázquez G, Reiter RJ, Agil A (2018) Melatonin increases brown adipose tissue mass and functionality in Zücker diabetic fatty rats: implications for obesity control. J. Pineal Res. 64 (4): e12472. doi: 10.1111/jpi.12472.
95. Jiménez-Aranda A, Fernández-Vázquez G, Campos D, Tassi M, Velasco-Perez L, Tan DX, Reiter RJ, Agil A (2013)Melatonin induces browning of inguinal white adipose tissue in Zucker diabetic fatty rats. J. Pineal Res. 55 (4): 416-423. doi: 10.1111/jpi.12089.
96. Agil A, Reiter RJ, Jiménez-Aranda A, Ibán-Arias R, Navarro-Alarcón M, Marchal JA, Adem A, Fernández-Vázquez G (2013) Melatonin ameliorates low-grade inflammation and oxidative stress in young Zucker diabetic fatty rats. J. Pineal Res. 54 (4): 381-388. doi: 10.1111/jpi.12012.
97. Jimenéz-Aranda A, Fernández-Vázquez G, Serrano MM, Reiter RJ, Agil A. 2014. Melatonin improves mitochondrial function in inguinal white adipose tissue of Zücker diabetic fatty rats. J. Pineal Res. 57 (1): 103-109. doi: 10.1111/jpi.12147.
98. Agil A, Rosado I, Ruiz R, Figaruea A, Nourlahuoda, Fernández Vázquez G. 2012. Melatonin improves glucose homeostasis in young Zucker diabetic fatty rats. J. Pineal Res. 52 (2): 203-210. doi: 10.1111/j.1600-079X.2011.00928.x.
99. Szewczyk-Golec K, Woźniak A, Reiter RJ (2015) Inter-relationships of the chronobiotic, melatonin, with leptin and adiponectin: implications for obesity. J. Pineal Res. 59 (3): 277-291. doi: 10.1111/jpi.12257.
100. Gonciarz M, Bielański W, Partyka R, Brzozowski T, Konturek PC, Eszyk J, Celiński K, Reiter RJ, Konturek SJ (2013) J. Pineal Res.54 (2): 154-161. doi:10.1111/j.1600-079X.2012.01023.x.
101. Koziróg M, Poliwczak AR, Duchnowicz P, Koter-Michalak M, Sikora J, Broncel M (2011) Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J. Pineal Res. 50 (3): 261-266. doi: 10.1111/j.1600-079X.2010.00835.x.
102. Bonnefont-Rousselot D (2014) Obesity and oxidative stress: potential roles of melatonin as antioxidant and metabolic regulator. Endocr. Metab. Immune Disord. Drug Targets 14 (3):159-168. PMID: 24934925.
103. Cano P, DP, Ríos‐Lugo MJ, Fernández‐Mateos MP, Reyes Toso CF, Esquifino AI (2012) Effect of a high‐fat diet on 24‐hour pattern of circulating adipocytokines in rats. Obesity 17 (10): 1866-1871. https://doi.org/10.1038/oby.2009.200.
104. Reiter RJ, Tan DX (2003) Melatonin: a novel protective agent against oxidative injury of the ischemic/reperfused heart. Cardiovasc. Res. 58 (1): 10-9. https://doi.org/10.1016/S0008-6363(02)00827-1.
105. Mukherjee D, Ghosh AK, Bandyopadhyay A, Basu A, Datta S, Pattari SK, Reiter RJ, Bandyopadhyay D (2012) Melatonin protects against isoproterenol-induced alterations in cardiac mitochondrial energy-metabolizing enzymes, apoptotic proteins, and assists in complete recovery from myocardial injury in rats. J. Pineal Res. 53 (2): 166-179. https://doi.org/10.1111/j.1600-079X.2012.00984.x.
106. Mukherjee D, Ghosh AK, Dutta M, Mitra E, Mallick S, Saha B, Reiter RJ, Bandyopadhyay D (2015) Mechanisms of isoproterenol-induced cardiac mitochondrial damage: protective actions of melatonin. J. Pineal Res. 58 (3): 275-290. doi: 10.1111/jpi.12213.
107. Liu Y, Li LN, Guo S, Zhao XY, Liu YZ, Liang C, Tu S, Wang D, Li L, Dong JZ, Gao L, Yang HB (2018) Melatonin improves cardiac function in a mouse model of heart failure with preserved ejection fraction. Redox Biol. 18: 211-221. doi: 10.1016/j.redox.2018.07.007.
108. Koh PO (2008) Melatonin regulates nitric oxide synthase expression in ischemic brain injury. J. Vet. Med. Sci. 70 (7): 747-750. doi: 10.1292/jvms.70.747.
109. Lim S, Park S (2014) Role of vascular smooth muscle cell in the inflammation of atherosclerosis. BMB Rep. 47 (1): 1-7. http://dx.doi.org/10.5483/BMBRep.2014.47.1.285.
110. Ma S, Chen J, Feng J, Zhang R, Fan M, Han D, Li X, Li C, Ren J, Wang Y, Cao F (2018) Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and nlrp3 inflammasome inhibition. Oxid. Med. Cell Longev. 2018: 9286458. doi: 10.1155/2018/9286458
111. Hu ZP, Fang XL, Fang N, Wang XB, Qian HY, Cao Z, Cheng Y, Wang BN, Wang Y (2013) Melatonin ameliorates vascular endothelial dysfunction, inflammation, and atherosclerosis by suppressing the TLR4/NF-κB system in high-fat-fed rabbits. J. Pineal Res. 55 (4): 388-398. doi:10.1111/jpi.12085.
112. Peterson JM, Seldin MM, Wei Z, Aja S, Wong GW (2013) CTRP3 attenuates diet-induced hepatic steatosis by regulating triglyceride metabolism. Am. J. Physiol. Gastrointest. Liver Physiol. 305 (3): G214-224. doi:10.1152/ajpgi.00102.2013.
113. Ma Q (2013) Role of nrf2 in oxidative stress and toxicity. Annu. Rev. Pharmacol. Toxicol. 53: 401-426. doi:10.1146/annurev-pharmtox-011112-140320.
114. Onyango P, Celic I, McCaffery JM, Boeke JD, Feinberg AP (2002) SIRT3, a human SIR2 homologue, is an NAD-dependent deacetylase localized to mitochondria. Proc. Natl. Acad. Sci. USA. 15: 99 (21):13653-13658. doi:10.1073/pnas.222538099.
115. Hirschey MD, Shimazu T, Jing E, Grueter CA, Collins AM, Aouizerat B, Stančáková A, Goetzman E, Lam MM, Schwer B, Stevens RD, Muehlbauer MJ, Kakar S, Bass NM, Kuusisto J, Laakso M, Alt FW, Newgard CB, Farese RV Jr, Kahn CR, Verdin E (2011) SIRT3 deficiency and mitochondrial protein hyperacetylation accelerate the development of the metabolic syndrome. Mol. Cell 44 (2): 177-190. doi:10.1016/j.molcel.2011.07.019.
116. Newsom SA, Boyle KE, Friedman JE (2013) Sirtuin 3: A major control point for obesity-related metabolic diseases? Drug Discov. Today Dis. Mech. 10 (1-2): e35-e40. doi:10.1016/j.ddmec.2013.04.001.
117. Schlicker C, Gertz M, Papatheodorou P, Kachholz B, Becker CF, Steegborn C (2008) Substrates and regulation mechanisms for the human mitochondrial sirtuins Sirt3 and Sirt5. J. Mol. Biol. 382 (3): 790-801. doi: 10.1016/j.jmb.2008.07.048.
118. Zhang M, Lin J, Wang, Cheng Z, Hu J, Wang T, Man W, Yin T, Guo W, Gao E, Reiter RJ, Wang H, Sun D (2017) Melatonin protects against diabetic cardiomyopathy through Mst1/Sirt3 signaling. J. Pineal Res. 63 (2). doi:10.1111/jpi.12418.
119. Zhai M, Li B, Duan W, Jing L, Zhang B, Zhang M, Yu L, Liu Z, Yu B, Ren K, Gao E, Yang Y, Liang H, Jin Z, Yu S (2017) Melatonin ameliorates myocardial ischemia reperfusion injury through SIRT3-dependent regulation of oxidative stress and apoptosis. J. Pineal Res. 63 (2): doi:10.1111/jpi.12419.
120. Kaskar, Rafee'ah (2015) Effect of melatonin on myocardial susceptibility to ischaemia and reperfusion damage in a rat model of high-fat diet-induced obesity.Thesis (MScMedSc)- Stellenbosch University. http://scholar.sun.ac.za/handle/10019.1/97868.
121. Nduhirabandi F, Du Toit EF, Blackhurst D, Marais D, Lochner A (2011) Chronic melatonin consumption prevents obesity-related metabolic abnormalities and protects the heart against myocardial ischemia and reperfusion injury in a prediabetic model of diet-induced obesity. J. Pineal Res. 50 (2): 171-182. doi:10.1111/j.1600-079X.2010.00826.x.
122. Nduhirabandi F, Huisamen B, Strijdom H, Blackhurst D, Lochner A (2014) Short-term melatonin consumption protects the heart of obese rats independent of body weight change and visceral adiposity. J. Pineal Res. 57 (3): 317-332. doi:10.1111/jpi.12171.
123. Miura T, Tanno M (2012) The mPTP and its regulatory proteins: final common targets of signalling pathways for protection against necrosis. Cardiovasc. Res. 94 (2): 181-189. doi:10.1093/cvr/cvr302.
124. Siasos G, Tsigkou V, Kosmopoulos M, Theodosiadis D, Simantiris S, Tagkou NM, Tsimpiktsioglou A, Stampouloglou PK, Oikonomou E, Mourouzis K, Philippou A, Vavuranakis M, Stefanadis C, Tousoulis D, Papavassiliou AG (2018) Mitochondria and cardiovascular diseases-from pathophysiology to treatment. Ann. Transl. Med. 6 (12): 256. doi: 10.21037/atm.2018.06.21.
125. Stacchiotti A, Favero G, Giugno L, Golic I, Korac A, Rezzani R (2017) Melatonin efficacy in obese leptin-deficient mice heart. Nutrients 9 (12): 1323. doi: https://doi.org/10.3390/nu9121323.
126. Potes Y, de Luxán-Delgado B, Rubio-González A, Reiter RJ and Coto Montes A (2019) Dose-dependent beneficial effect of melatonin on obesity; interaction of melatonin and leptin. Melatonin Res. 2 (1): 1-8. DOI:https://doi.org/https://doi.org/10.32794/mr11250008.
127. Murphy E, Steenbergen C (2008) Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol. Rev. 88 (2): 581-609. doi: 10.1152/physrev.00024.2007.
128. Kroemer G, Galluzzi L, Brenner C (2007) Mitochondrial membrane permeabilization in cell death. Physiol. Rev. 87 (1): 99-163. doi:10.1152/physrev.00013.2006.
129. Littlejohns B, Pasdois P, Duggan S, Bond AR, Heesom K, Jackson CL, Angelini GD, Halestrap AP, Suleiman MS (2014) Hearts from mice fed a non-obesogenic high-fat diet exhibit changes in their oxidative state, calcium and mitochondria in parallel with increased susceptibility to reperfusion injury. PLoS One 9 (6): e100579. doi: 10.1371/journal.pone.0100579.
130. Petrosillo G, Colantuono G, Moro N, Ruggiero FM, Tiravanti E, Di Venosa N, Fiore T, Paradies G (2009) Am. J. Physiol. Heart Circ. Physiol. 297 (4): H1487-H1493. doi:10.1152/ajpheart.00163.2009.
131. Tan DX, Zanghi B, Lucien MC, Reiter RJ (2014) Melatonin identified in meats and other food stuffs: Potentially nutritional impact. J. Pineal Res. 57 (2): 213-218. doi: 10.1111/jpi.12152.
132. Peuhkuri K, Sihvola N, Korpela R (2012) Dietary factors and fluctuating levels of melatonin. Food Nutr. Res. 56: 17252. doi:10.3402/fnr.v56i0.17252.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.