Multiple strategies of melatonin protecting against cardiovascular injury related to inflammation: A comprehensive overview
Melatonin in inflammatory cardiovascular injury
Abstract
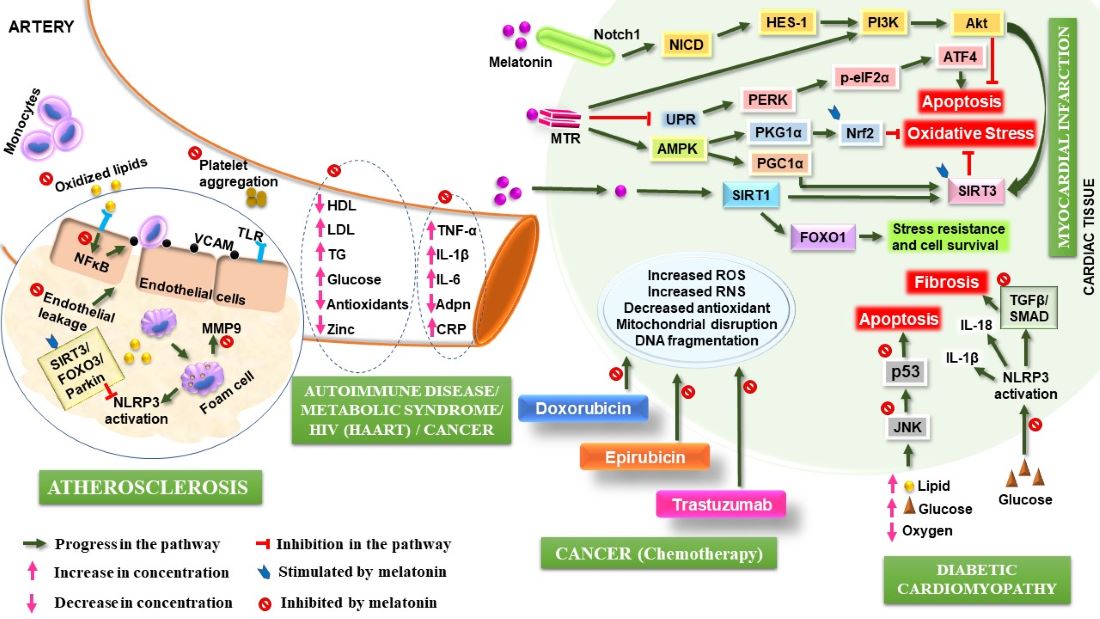
The onset and progression of baneful chronic diseases are often accompanied by a torrent of uncontrolled inflammatory reactions. Although inflammation is a natural response to detect, eliminate, and counterpoise the harmful insults to physiological integrity, a persistent inflammation causes tissue damage or more serious disorders, for example, the atherosclerosis and myocardial infarction. Inflammation often occurs in the cardiovascular system, but are also caused by other disorders including metabolic syndrome, autoimmune diseases, AIDS, and cancer that can affect the cardiac health. To effectively treat heart diseases a potent remedy is necessary which not only suppresses the inflammation but also prevents inflammation-associated cardio-pathogenesis. The ubiquitous antioxidant molecule melatonin has both anti-inflammatory and cardioprotective activities. Melatonin executes its anti-inflammatory activity by its antioxidant function or by targeting multiple intracellular signalling cascades such as modulating cytokine profile, blocking inflammasome activation and apoptosis. Lipid dysregulation and endothelial dysfunction that play a crucial role in the pathogenesis of atherosclerosis, insulin resistance, and diabetes are prevented by melatonin. Attenuation of mitochondrial and ER stress by melatonin is also pertinent to its cardioprotective action. Additionally, melatonin by its immuno-stimulatory activity can suppress inflammaging and immuno-senescence in HIV patients and thereby averts chronic inflammation-induced cardiovascular abnormality in these subjects. Modulation of cytokine profile and decrease in MMP-9 secretion by melatonin is beneficial in autoimmune conditions. In addition to its anti-tumour potency, melatonin can reduce chemotherapy-induced cardio-toxicity in cancer patients. This review, therefore, provides a concise summary of the currently available information appertaining to the roles of melatonin in mitigation of chronic inflammation and its effect on cardiovascular integrity.
References
2. Welsh P, Grassia G, Botha S, Sattar N, Maffia P (2017) Targeting inflammation to reduce cardiovascular disease risk: a realistic clinical prospect?. Br. J. Pharmacol. 174: 3898-3913. DOI: 10.1111/bph.13818.
3. Geovanini GR, Libby P (2018) Atherosclerosis and inflammation: overview and updates. Clin. Sci. 132: 1243-1252. DOI: 10.1042/CS20180306.
4. Parekh RS, Plantinga LC, Kao WL, Meoni LA, Jaar BG, Fink NE, Powe NR, Coresh J, Klag MJ (2008) The association of sudden cardiac death with inflammation and other traditional risk factors. Kidney Int. 74: 1335-1342. DOI: 10.1038/ki.2008.449.
5. Ma Z, Xu L, Liu D, Zhang X, Di S, Li W, Zhang J, Reiter RJ, Han J, Li X, Yan X (2020) Utilizing melatonin to alleviate side effects of chemotherapy: a potentially good partner for treating cancer with ageing. Oxid. Med. Cell Longev. 2020: 6841581. DOI: 10.1155/2020/6841581.
6. Mendes AF, Cruz MT, Gualillo O (2018) The Physiology of inflammation–the final common pathway to disease. Front. Physiol. 9: 1741. DOI: 10.3389/fphys.2018.01741.
7. Biswas SK (2016) Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid. Med. Cell Longev. 2016: 5698931. DOI: 10.1155/2016/5698931.
8. Radogna F, Diederich M, Ghibelli L (2010) Melatonin: a pleiotropic molecule regulating inflammation. Biochem. Pharmacol. 80: 1844-1852. DOI: 10.1016/j.bcp.2010.07.041.
9. Cipolla-Neto J, Amaral FG (2018) Melatonin as a hormone: new physiological and clinical insights. Endocr. Rev. 39: 990-1028. DOI: 10.1210/er.2018-00084.
10. Ekmekcioglu C, Thalhammer T, Humpeler S, Mehrabi MR, Glogar HD, Hölzenbein T, Markovic O, Leibetseder VJ, Strauss‐Blasche G, Marktl W (2003) The melatonin receptor subtype MT2 is present in the human cardiovascular system. J. Pineal Res. 35: 40-44. DOI: 10.1034/j.1600-079x.2003.00051.x.
11. Slominski RM, Reiter RJ, Schlabritz-Loutsevitch N, Ostrom RS, Slominski AT (2012) Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol. Cell. Endocrinol. 351: 152-166. DOI: 10.1016/j.mce.2012.01.004.
12. Nabavi SM, Nabavi SF, Sureda A, Xiao J, Dehpour AR, Shirooie S, Silva AS, Baldi A, Khan H, Daglia M (2019) Anti-inflammatory effects of Melatonin: A mechanistic review. Crit. Rev. Food Sci. Nutr. 59: S4-S16. DOI: 10.1080/10408398.2018.1487927.
13. Mauriz JL, Collado PS, Veneroso C, Reiter RJ, González‐Gallego J (2013) A review of the molecular aspects of melatonin’s anti‐inflammatory actions: recent insights and new perspectives. J. Pineal Res. 54: 1-4. Doi:10.1111/j.1600-079X.2012.01014.x.
14. Tan DX, Reiter RJ, Manchester LC, Yan MT, El-Sawi M, Sainz RM, Mayo JC, Kohen R, Allegra MC, Hardeland R (2002) Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr. Top. Med. Chem. 2: 181-197. DOI: 10.2174/1568026023394443.
15. Reiter RJ, Tan DX, Kim SJ, Qi W (1998) Melatonin as a pharmacological agent against oxidative damage to lipids and DNA. Proc. West Pharmacol. Soc. 41: 229–236.
16. Favero G, Franceschetti L, Bonomini F, Rodella LF, Rezzani R (2017) Melatonin as an anti-inflammatory agent modulating inflammasome activation. Int. J. Endocrinol. 2017: 1835195. DOI: 10.1155/2017/1835195.
17. Reiter RJ, Calvo JR, Karbownik M, Qi W, Tan DX (2000) Melatonin and its relation to the immune system and inflammation. Ann. N. Y. Acad. Sci. 917: 376-386. DOI: 10.1111/j.1749-6632.2000.tb05402.x.
18. Carrillo‐Vico A, Lardone PJ, Naji L, Fernández‐Santos JM, Martín‐Lacave I, Guerrero JM, Calvo JR (2005) Beneficial pleiotropic actions of melatonin in an experimental model of septic shock in mice: regulation of pro-/anti-inflammatory cytokine network, protection against oxidative damage and anti-apoptotic effects. J. Pineal Res. 39: 400-408. DOI: 10.1111/j.1600-079X.2005.00265.x.
19. Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L (2018) Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 9: 7204–7218. DOI: 10.18632/oncotarget.23208.
20. Brusselle G, Bracke K (2014) Targeting immune pathways for therapy in asthma and chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 11: S322-S328. DOI: 10.1513/AnnalsATS.201403-118AW.
21. Gudkov AV, Komarova EA (2016) p53 and the Carcinogenicity of chronic inflammation. Cold Spring Harb. Perspect. Med .6: a026161 DOI: 10.1101/cshperspect.a026161.
22. Janeway CA Jr, Medzhitov R (2002) Innate immune recognition. Annu. Rev. Immunol. 20: 197-216. DOI: 10.1146/annurev.immunol.20.083001.084359.
23. Yamamoto M, Takeda K (2010) Current views of toll-like receptor signaling pathways. Gastroenterol. Res. Pract. 2010: 240365. DOI: 10.1155/2010/240365.
24. Kawasaki T, Kawai T (2014) Toll-like receptor signaling pathways. Front. Immunol.5: 461. DOI: 10.3389/fimmu.2014.00461.
25. Jaffer U, Wade RG, Gourlay T (2010) Cytokines in the systemic inflammatory response syndrome: a review. HSR Proc. Intensive Care Cardiovasc. Anesth. 2: 161.
26. Mokart D, Capo C, Blache JL, Delpero JR, Houvenaeghel G, Martin C, Mege JL (2002) Early postoperative compensatory anti‐inflammatory response syndrome is associated with septic complications after major surgical trauma in patients with cancer. Br. J. Surg. 89: 1450-1456. DOI: 10.1046/j.1365-2168.2002.02218.x.
27. Halter J, Steinberg J, Fink G, Lutz C, Picone A, Maybury R, Fedors N, DiRocco J, Lee HM, Nieman G (2005) Evidence of systemic cytokine release in patients undergoing cardiopulmonary bypass. J. Extra Corpor. Technol. 37: 272-277.
28. Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB (2010) Oxidative stress, inflammation, and cancer: how are they linked? Free Radic. Biol. Med. 49: 1603-1616. DOI: 10.1016/j.freeradbiomed.2010.09.006.
29. Pereira EJ, Smolko CM, Janes KA (2016) Computational models of reactive oxygen species as metabolic byproducts and signal-transduction modulators. Front. Pharmacol. 7: 457. DOI: 10.3389/fphar.2016.00457.
30. Smith DA, Germolec DR (1999) Introduction to immunology and autoimmunity. Environ. Health Perspect. 107: 661-665. DOI: 10.1289/ehp.99107s5661.
31. Yamamoto K (2004) Mechanisms of autoimmunity. Autoimmune Dis. 47: 403–406.
32. Rosenblum MD, Remedios KA, Abbas AK (2015) Mechanisms of human autoimmunity. J. Clin. Invest. 125: 2228-2233. DOI: 10.1172/JCI78088.
33. Appay V, Almeida JR, Sauce D, Autran B, Papagno L (2007) Accelerated immune senescence and HIV-1 infection. Exp. Gerontol. 42: 432-437. DOI: 10.1016/j.exger.2006.12.003.
34. Sereti I, Altfeld M (2016) Immune activation and HIV: an enduring relationship. Curr. Opin. HIV AIDS 11: 129-130. DOI: 10.1097/COH.0000000000000244.
35. Hatano H (2013) Immune activation and HIV persistence: considerations for novel therapeutic interventions. Curr. Opin. HIV AIDS 8: 211-216. DOI: 10.1097/COH.0b013e32835f9788.
36. Miller CJ, Baker JV, Bormann AM, Erlandson KM, Hullsiek KH, Justice AC, Neuhaus J, Paredes R, Petoumenos K, Wentworth D, Winston A (2014) Adjudicated morbidity and mortality outcomes by age among individuals with HIV infection on suppressive antiretroviral therapy. PloS One 9: e95061 DOI: 10.1371/journal.pone.0095061.
37. Bucy RP, Hockett RD, Derdeyn CA, Saag MS, Squires K, Sillers M, Mitsuyasu RT, Kilby JM (1999) Initial increase in blood CD4+ lymphocytes after HIV antiretroviral therapy reflects redistribution from lymphoid tissues. J. Clin. Invest. 103: 1391-1398. DOI: 10.1172/JCI5863.
38. Cohen Stuart JW, Hazebergh MD, Hamann D, Otto SA, Borleffs JC, Miedema F, Boucher CA, de Boer RJ (2000) The dominant source of CD4+ and CD8+ T-cell activation in HIV infection is antigenic stimulation. J. Acquir. Immune Defic. Syndr. 25: 203-211. DOI: 10.1097/00042560-200011010-00001.
39. Wolf K, Tsakiris DA, Weber R, Erb P, Battegay M, Swiss HIV cohort study (2002) Antiretroviral therapy reduces markers of endothelial and coagulation activation in patients infected with human immunodeficiency virus type 1. J. Infect. Dis. 185: 456-462. DOI: 10.1086/338572.
40. Malherbe G, Steel HC, Cassol S, De Oliveira T, Seebregts CJ, Anderson R, Cassol E, Rossouw TM (2014) Circulating biomarkers of immune activation distinguish viral suppression from nonsuppression in HAART-treated patients with advanced HIV-1 subtype C infection. Mediators Inflamm. 2014: 198413. DOI: 10.1155/2014/198413.
41. Sokoya T, Steel HC, Nieuwoudt M, Rossouw TM (2017) HIV as a cause of immune activation and immunosenescence. Mediators Inflamm. 2017: 6825493. DOI: 10.1155/2017/6825493.
42. Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet. Med. 15: 539-553. DOI: https://apps.who.int/iris/handle/10665/66040.
43. Boden G, Shulman GI (2002) Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and β‐cell dysfunction. Eur. J. Clin. Invest. 32: 14-23.
44. Tooke JE, Hannemann MM (2000) Adverse endothelial function and the insulin resistance syndrome. Journal of internal medicine. 247: 425-431. DOI: 10.1046/j.1365-2362.32.s3.3.x.
45. Di Lorenzo C, Dell'Agli M, Colombo E, Sangiovanni E, Restani P (2013) Metabolic syndrome and inflammation: a critical review of in vitro and clinical approaches for benefit assessment of plant food supplements. Evid. Based Complement. Alternat. Med. 2013: 782461. DOI: 10.1155/2013/782461.
46. Barchetta I, Cimini FA, Ciccarelli G, Baroni MG, Cavallo MG (2019) Sick fat: the good and the bad of old and new circulating markers of adipose tissue inflammation. J. Endocrinol. Invest. 42: 1257-1272. DOI: 10.1007/s40618-019-01052-3.
47. Reddy P, Lent-Schochet D, Ramakrishnan N, McLaughlin M, Jialal I (2019) Metabolic syndrome is an inflammatory disorder: A conspiracy between adipose tissue and phagocytes. Clin. Chim. Acta. 496: 35-44. DOI: 10.1016/j.cca.2019.06.019.
48. Hotamisligil GS, Murray DL, Choy LN, Spiegelman BM (1994) Tumor necrosis factor alpha inhibits signaling from the insulin receptor. Proc. Natl. Acad. Sci. 91: 4854-4858. DOI: 10.1073/pnas.91.11.4854.
49. Rochlani Y, Pothineni NV, Kovelamudi S, Mehta JL (2017) Metabolic syndrome: pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 11: 215-225. DOI: 10.1177/1753944717711379.
50. Fried SK, Bunkin DA, Greenberg AS (1998) Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: depot difference and regulation by glucocorticoid. J. Clin. Endocrinol. Metab .83: 847-850. DOI: 10.1210/jcem.83.3.4660.
51. Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357: 539-545. DOI: 10.1016/S0140-6736(00)04046-0.
52. Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454: 436-444. DOI: https://doi.org/10.1038/nature07205.
53. Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420: 860-867. DOI: https://doi.org/10.1038/nature01322
54. Brigati C, Noonan DM, Albini A, Benelli R (2002) Tumors and inflammatory infiltrates: friends or foes? Clin. Exp. Metastasis 19: 247-258. DOI: 10.1023/a:1015587423262.
55. Tsung K, Dolan JP, Tsung YL, Norton JA (2002) Macrophages as effector cells in interleukin 12-induced T cell-dependent tumor rejection. Cancer Res. 62: 5069-5075.
56. Torisu H, Ono M, Kiryu H, Furue M, Ohmoto Y, Nakayama J, Nishioka Y, Sone S, Kuwano M (2000) Macrophage infiltration correlates with tumor stage and angiogenesis in human malignant melanoma: possible involvement of TNFα and IL-1α. Int. J. Cancer 85: 182-188. DOI: 10.1002/(SICI)1097-0215(20000115)85:23.0.CO;2-M.
57. Schoppmann SF, Birner P, Stöckl J, Kalt R, Ullrich R, Caucig C, Kriehuber E, Nagy K, Alitalo K, Kerjaschki D (2002) Tumor-associated macrophages express lymphatic endothelial growth factors and are related to peritumoral lymphangiogenesis. Am. J. Pathol. 161: 947-956. DOI: 10.1016/S0002-9440(10)64255-1.
58. Collins T, Cybulsky MI (2001) NF-κB: pivotal mediator or innocent bystander in atherogenesis? J. Clin. Invest. 107: 255-264. DOI: 10.1172/JCI10373.
59. Khan BV, Parthasarathy SS, Alexander RW, Medford RM (1995) Modified low-density lipoprotein and its constituents augment cytokine-activated vascular cell adhesion molecule-1 gene expression in human vascular endothelial cells. J. Clin. Invest. 95: 1262-1270. DOI: 10.1172/JCI117776.
60. Palmetshofer A, Robson SC, Nehls V (1999) Lysophosphatidic acid activates nuclear factor kappa B and induces proinflammatory gene expression in endothelial cells. Thromb. Haemost. 82: 1532-1537. DOI: 10.1055/s-0037-1614867.
61. Dichtl W, Nilsson L, Goncalves I, Ares MP, Banfi C, Calara F, Hamsten A, Eriksson P, Nilsson J (1999) Very low-density lipoprotein activates nuclear factor-kappaB in endothelial cells. Circ. Res. 84: 1085-1094. DOI: https://doi.org/10.1161/01.RES.84.9.1085.
62. Libby P (2002) Inflammation in atherosclerosis. Nature 420: 868–874. DOI: https://doi.org/10.1038/nature01323.
63. Mach F, Sauty A, Iarossi AS, Sukhova GK, Neote K, Libby P, Luster AD (1999) Differential expression of three T lymphocyte-activating CXC chemokines by human atheroma-associated cells. J. Clin. Invest. 104: 1041–1050. DOI: 10.1172/JCI6993.
64. Frangogiannis NG, Smith CW, Entman ML (2002) The inflammatory response in myocardial infarction. Cardiovasc. Res. 53: 31-47. DOI: 10.1016/s0008-6363(01)00434-5.
65. Liu J, Wang H, Li J (2016) Inflammation and inflammatory cells in myocardial infarction and reperfusion injury: a double-edged sword. Clin. Med. Insights Cardiol. 10: 79-84. DOI: 10.4137/CMC.S33164.
66. Pfeffer MA, Braunwald E (1990) Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation 81: 1161–1172. DOI: 10.1161/01.cir.81.4.1161.
67. Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA (2006) Controversies in ventricular remodelling. Lancet 367: 356–367. DOI: 10.1016/S0140-6736(06)68074-4.
68. Ong SB, Hernández-Reséndiz S, Crespo-Avilan GE, Mukhametshina RT, Kwek XY, Cabrera-Fuentes HA, Hausenloy DJ (2018) Inflammation following acute myocardial infarction: multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol. Ther. 186: 73-87. DOI: 10.1016/j.pharmthera.2018.01.001.
69. Marchant DJ, Boyd JH, Lin DC, Granville DJ, Garmaroudi FS, McManus BM (2012) Inflammation in myocardial diseases. Circ. Res. 110: 126–144. DOI: 10.1161/CIRCRESAHA.111.243170.
70. van Hout GP, Arslan F, Pasterkamp G, Hoefer IE (2016) Targeting danger-associated molecular patterns after myocardial infarction. Expert Opin. Ther. Targets 20: 223–239. DOI: 10.1517/14728222.2016.1088005.
71. Timmers L, Pasterkamp G, de Hoog VC, Arslan F, Appelman Y, de Kleijn DP (2012) The innate immune response in reperfused myocardium. Cardiovasc. Res. 94: 276–283. DOI: 10.1093/cvr/cvs018.
72. Roman MJ, Moeller E, Davis A, Paget SA, Crow MK, Lockshin MD, Sammaritano L, Devereux RB, Schwartz JE, Levine DM, Salmon JE (2006) Preclinical carotid atherosclerosis in patients with rheumatoid arthritis. Ann. Intern. Med. 144: 249-256. DOI: 10.7326/0003-4819-144-4-200602210-00006.
73. Gonzalez A, Maradit Kremers H, Crowson CS, Nicola PJ, Davis III JM, Therneau TM, Roger VL, Gabriel SE (2007) The widening mortality gap between rheumatoid arthritis patients and the general population. Arthritis Rheum. 56: 3583-3587. DOI: 10.1002/art.22979.
74. Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D (2012) Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann. Rheum. Dis. 71: 1524-1529. DOI: 10.1136/annrheumdis-2011-200726.
75. Devlin CM, Kuriakose G, Hirsch E, Tabas I (2002) Genetic alterations of IL-1 receptor antagonist in mice affect plasma cholesterol level and foam cell lesion size. Proc. Natl. Acad. Sci. 99: 6280-6285. DOI: 10.1073/pnas.092324399.
76. Ohta H, Wada H, Niwa T, Kirii H, Iwamoto N, Fujii H, Saito K, Sekikawa K, Seishima M (2005) Disruption of tumor necrosis factor-α gene diminishes the development of atherosclerosis in ApoE-deficient mice. Atherosclerosis 180: 11-17. DOI: 10.1016/j.atherosclerosis.2004.11.016.
77. Chuang YW, Yu MC, Lin CL, Yu TM, Shu KH, Kao CH (2015) Risk of peripheral arterial occlusive disease in patients with systemic lupus erythematosus: a nationwide population-based cohort study. Medicine 94: e2121. DOI: 10.1097/MD.0000000000002121.
78. Holmqvist M, Simard JF, Asplund K, Arkema EV (2015) Stroke in systemic lupus erythematosus: a meta-analysis of population-based cohort studies. RMD Open 1: e000168. DOI: 10.1136/rmdopen-2015-000168.
79. Kay SD, Poulsen MK, Diederichsen AC, Voss A (2016) Coronary, carotid, and lower-extremity atherosclerosis and their interrelationship in Danish patients with systemic lupus erythematosus. J. Rheumatol. 43: 315-322. DOI: 10.3899/jrheum.150488.
80. Meune C, Khanna D, Aboulhosn J, Avouac J, Kahan A, Furst DE, Allanore Y (2016) A right ventricular diastolic impairment is common in systemic sclerosis and is associated with other target-organ damage. Semin. Arthritis Rheum. 45: 439-445. DOI: 10.1016/j.semarthrit.2015.07.002.
81. Aniwan S, Pardi DS, Tremaine WJ, Loftus EV (2018) Increased risk of acute myocardial infarction and heart failure in patients with inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 16: 1607–1615. DOI: 10.1016/j.cgh.2018.04.031.
82. Bigeh A, Sanchez A, Maestas C, Gulati M (2019) Inflammatory bowel disease & the risk for cardiovascular disease: does all inflammation lead to heart disease?. Trends Cardiovasc. Med. S1050-1738 (19): 30139-30142. DOI: 10.1016/j.tcm.2019.10.001.
83. Plevy S, Silverberg MS, Lockton S, Stockfisch T, Croner L, Stachelski J, Brown M, Triggs C, Chuang E, Princen F, Singh S (2013) Combined serological, genetic, and inflammatory markers differentiate non-IBD, Crohn’s disease, and ulcerative colitis patients. Inflamm. Bowel Dis. 19: 1139–1148. DOI: 10.1097/MIB.0b013e318280b19e.
84. Ridker PM, Wilson PW, Grundy SM (2004) Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk?. Circulation 109: 2818–2825. DOI: 10.1161/01.CIR.0000132467.45278.59.
85. Mehta PK, Griendling KK (2007) Angiotensin II cell signaling: physiological and pathological effects in the cardiovascular system. Am. J. Physiol. Cell Physiol. 292: C82–C97. DOI: 10.1152/ajpcell.00287.2006.
86. Fitzpatrick T, Carrier M, Le Gal G (2017) Cancer, atrial fibrillation, and stroke. Thromb. Res. 155: 101-105. DOI: 10.1016/j.thromres.2017.05.006.
87. Lo J, Abbara S, Shturman L, Soni A, Wei J, Rocha-Filho JA, Nasir K, Grinspoon SK (2010) Increased prevalence of subclinical coronary atherosclerosis detected by coronary computed tomography angiography in HIV-infected men. AIDS 24: 243-253. DOI: 10.1097/QAD.0b013e328333ea9e.
88. Dinarello CA (2010) Anti-inflammatory agents: present and future. Cell 140: 935-950. DOI: 10.1016/j.cell.2010.02.043.
89. Henson PM (2005) Dampening inflammation. Nat. Immunol. 6: 1179-1181. DOI: 10.1038/ni1205-1179.
90. Serhan CN, Brain SD, Buckley CD, Gilroy DW, Haslett C, O'Neill LA, Perretti M, Rossi AG, Wallace JL (2007) Resolution of inflammation: state of the art, definitions and terms. FASEB J. 21: 325-332. DOI: 10.1096/fj.06-7227rev.
91. Freire MO, Van Dyke TE (2013) Natural resolution of inflammation. Periodontol. 2000.? 63: 149-164. DOI: 10.1111/prd.12034.
92. Bannenberg G, Serhan CN (2010) Specialized pro-resolving lipid mediators in the inflammatory response: An update. Biochim. Biophys. Acta 1801: 1260–1273. DOI: 10.1016/j.bbalip.2010.08.002.
93. Bannenberg GL, Chiang N, Ariel A, Arita M, Tjonahen E, Gotlinger KH, Hong S, Serhan CN (2005) Molecular circuits of resolution: formation and actions of resolvins and protectins. J. Immunol. 174: 4345–4355. DOI: 10.4049/jimmunol.174.7.4345.
94. Hasturk H, Kantarci A, Goguet-Surmenian E, Blackwood A, Andry C, Serhan CN, Van Dyke TE (2007) Resolvin E1 regulates inflammation at the cellular and tissue level and restores tissue homeostasis in vivo. J. Immunol. 179: 7021–7029. DOI: 10.4049/jimmunol.179.10.7021.
95. Samuelsson B, Dahlen SE, Lindgren JA, Rouzer CA, Serhan CN (1987) Leukotrienes and lipoxins: structures, biosynthesis, and biological effects. Science 237: 1171–1176. DOI: 10.1126/science.2820055.
96. Maddox JF, Colgan SP, Clish CB, Petasis NA, Fokin VV, Serhan CN (1998) Lipoxin B4 regulates human monocyte/neutrophil adherence and motility: design of stable lipoxin B4 analogs with increased biologic activity. FASEB J. 12: 487–494 DOI: 10.1096/fasebj.12.6.487.
97. Lerner AB, Case JD, Takahashi Y, Lee TH, Mori W (1958) Isolation of melatonin, the pineal gland factor that lightens melanocytes. J. Am. Chem. Soc .80: 2587. DOI: https://doi.org/10.1021/ja01543a060.
98. Lerner AB, Case JD, Heinzelmann RV (1959) Structure of melatonin. J. Am. Chem. Soc. 81: 6084-6085. DOI: https://doi.org/10.1021/ja01531a060.
99. Zhao D, Yu Y, Shen Y, Liu Q, Zhao Z, Sharma R, Reiter RJ (2019) Melatonin synthesis and function: evolutionary history in animals and plants. Front. Endocrinol. 10: 249. DOI: 10.3389/fendo.2019.00249.
100. Cardinali, D. P., Pandi-Perumal, S. R., & Niles, L. P (2008) Melatonin and its receptors: biological function in circadian sleep-wake regulation (Cambridge University Press, Cambridge), pp 283-314. DOI: 10.1017/CBO9780511541674.011.
101. Tan DX, Manchester LC, Hardeland R, Lopez‐Burillo S, Mayo JC, Sainz RM, Reiter RJ (2003) Melatonin: a hormone, a tissue factor, an autocoid, a paracoid, and an antioxidant vitamin. J. Pineal Res. 34: 75-78. DOI: 10.1034/j.1600-079x.2003.02111.x.
102. Reiter RJ, Mayo JC, Tan DX, Sainz RM, Alatorre‐Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61: 253-278. DOI: 10.1111/jpi.12360.
103. Carrillo-Vico A, Reiter RJ, Lardone PJ, Herrera JL, Fernández-Montesinos R, Guerrero JM, Pozo D (2006) The modulatory role of melatonin on immune responsiveness. Curr. Opin. Investig. Drugs 7: 423.
104. Hardeland R (2018) Melatonin and inflammation—Story of a double‐edged blade. J. Pineal Res. 65: e12525. DOI: 10.1111/jpi.12525.
105. Galano A, Tan DX, Reiter RJ (2011) Melatonin as a natural ally against oxidative stress: a physicochemical examination. J. Pineal Res. 51: 1-6.
106. García JJ, López-Pingarrón L, Almeida-Souza P, Tres A, Escudero P, García-Gil FA, Tan DX, Reiter RJ, Ramírez JM, Bernal-Pérez M (2014) Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: a review. J. Pineal Res. 56: 225–237. DOI: 10.1111/jpi.12128.
107. Chelombitko MA (2018) Role of Reactive Oxygen Species in Inflammation: A Minireview. Moscow Univ. Biol. Sci. Bull. 73: 199–202. DOI: https://doi.org/10.3103/S009639251804003X.
108. Segal AW (2008) The function of the NADPH oxidase of phagocytes and its relationship to other NOXs in plants, invertebrates, and mammals. Int. J. Biochem. Cell 40: 604–618. DOI: 10.1016/j.biocel.2007.10.003.
109. Blasig IE, Bellmann C, Cording J, Del Vecchio G, Zwanziger D, Huber O, Haseloff RF (2011) Occludin protein family: Oxidative stress and reducing conditions. Antioxid. Redox. Signaling 15: 1195–1219. DOI: 10.1089/ars.2010.3542.
110. Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB (2008) Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox. Signaling 20: 1126–1167. DOI: 10.1089/ars.2012.5149.
111. Laurila JP, Laatikainen LE, Castellone MD, Laukkanen MO (2009) SOD3 reduces inflammatory cell migration by regulating adhesion molecule and cytokine expression. PLoS One 4: e5786. DOI: 10.1371/journal.pone.0005786.
112. Liu F, Ng TB (2000) Effect of pineal indoles on activities of the antioxidant defense enzymes superoxide dismutase, catalase, and glutathione reductase, and levels of reduced and oxidized glutathione in rat tissues. Biochem. Cell Biol. 78: 447-453. DOI: 10.1139/o00-018.
113. Pasparakis M, Luedde T, Schmidt-Supprian M (2006) Dissection of the NF-κB signalling cascade in transgenic and knockout mice. Cell Death Differ. 13: 861–872. DOI: 10.1038/sj.cdd.4401870.
114. Lawrence T (2009) The nuclear factor NF-κB pathway in inflammation. Cold Spring Harb. Perspect. Biol. 1: a001651. DOI: 10.1101/cshperspect.a001651.
115. García-Mediavilla V, Crespo I, Collado PS, Esteller A, Sánchez-Campos S, Tuñón MJ, González-Gallego J (2007) The anti-inflammatory flavones quercetin and kaempferol cause inhibition of inducible nitric oxide synthase, cyclooxygenase-2 and reactive C-protein, and down-regulation of the nuclear factor kappaB pathway in Chang Liver cells. Eur. J. Pharmacol. 557: 221-229. DOI: 10.1016/j.ejphar.2006.11.014.
116. Hayden MS, Ghosh S (2012) NF-κB, the first quarter-century: remarkable progress and outstanding questions. Gene Dev. 26: 203–234. DOI: 10.1101/gad.183434.111.
117. Cuesta S, Kireev R, Forman K, García C, Escames G, Ariznavarreta C, Vara E, Tresguerres JA (2010) Melatonin improves inflammation processes in liver of senescence-accelerated prone male mice (SAMP8). Exp. Gerontol. 45: 950–956. DOI: 10.1016/j.exger.2010.08.016.
118. Rodríguez-Reynoso S, Leal C, Portilla E, Olivares N, Muñiz J (2001) Effect of exogenous melatonin on hepatic energetic status during ischemia/reperfusion: possible role of tumor necrosis factoralpha and nitric oxide. J. Surg. Res. 100: 141–149. DOI: 10.1006/jsre.2001.6185.
119. Koh PO (2008) Melatonin regulates nitric oxide synthase expression in ischemic brain injury. J. Vet. Med. Sci. 70: 747–750. DOI: 10.1292/jvms.70.747.
120. Li Z, Nickkholgh A, Yi X, Bruns H, Gross ML, Hoffmann K, Mohr E, Zorn M, Büchler MW, Schemmer P (2009) Melatonin protects kidney grafts from ischemia/reperfusion injury through inhibition of NF-kB and apoptosis after experimental kidney transplantation. J. Pineal Res. 46: 365–372. DOI: 10.1111/j.1600-079X.2009.00672.x.
121. Alonso M, Collado PS, González‐Gallego J (2006) Melatonin inhibits the expression of the inducible isoform of nitric oxide synthase and nuclear factor kappa B activation in rat skeletal muscle. J. Pineal Res. 41: 8-14. DOI: 10.1111/j.1600-079X.2006.00323.x.
122. Veneroso C, Tuñón MJ, González‐Gallego J, Collado PS (2009) Melatonin reduces cardiac inflammatory injury induced by acute exercise. J. Pineal Res. 47: 184-191. DOI: 10.1111/j.1600-079X.2009.00699.x.
123. Rosales-Corral SA, Acuña-Castroviejo D, Coto-Montes A, Boga JA, Manchester LC, Fuentes-Broto L, Korkmaz A, Ma S, Tan DX, Reiter RJ (2012) Alzheimer’s disease: pathological mechanisms and the beneficial role of melatonin. J. Pineal Res. 52: 167–202. DOI: 10.1111/j.1600-079X.2011.00937.x.
124. Chen CF, Wang D, Reiter RJ, Yeh DY (2011) Oral melatonin attenuates lung inflammation and airway hyperreactivity induced by inhalation of aerosolized pancreatic fluid in rats. J. Pineal Res. 50: 46–53. DOI: 10.1111/j.1600-079X.2010.00808.x.
125. Cuzzocrea S, Mazzon E, Serraino I, Lepore V, Terranova ML, Ciccolo A, Caputi AP (2001) Melatonin reduces dinitrobenzene sulfonic acid-induced colitis. J. Pineal Res. 30: 1–12. DOI: 10.1034/j.1600-079x.2001.300101.x.
126. Negi G, Kumar A, Sharma SS (2011) Melatonin modulates neuroinflammation and oxidative stress in experimental diabetic neuropathy: effects on NF-kappaB and Nrf2 cascades. J. Pineal Res. 50: 124–131. DOI: 10.1111/j.1600-079X.2010.00821.x.
127. Martínez-Campa C, González A, Mediavilla MD, Alonso-González C, Alvarez-García V, Sánchez-Barceló EJ, Cos S (2009) Melatonin inhibits aromatase promoter expression by regulating cyclooxygenases expression and activity in breast cancer cells. Br. J. Cancer 101: 1613–1619. DOI: 10.1038/sj.bjc.6605336.
128. Kireev RA, Tresguerres AC, Garcia C, Ariznavarreta C, Vara E, Tresguerres JA (2008) Melatonin is able to prevent the liver of old castrated female rats from oxidative and pro-inflammatory damage. J. Pineal Res. 45: 394–402. DOI: 10.1111/j.1600-079X.2008.00606.x.
129. Forman K, Vara E, García C, Kireev R, Cuesta S, Escames G, Tresguerres JA (2011) Effect of a combined treatment with growth hormone and melatonin in the cardiological aging on male SAMP8 mice. J. Gerontol. A. Biol. Sci. Med. Sci. 66: 823–834. DOI: 10.1093/gerona/glr083.
130. Cuesta S, Kireev R, García C, Forman K, Escames G, Vara E, Tresguerres JA (2011) Beneficial effect of melatonin treatment on inflammation, apoptosis and oxidative stress on pancreas of a senescence accelerated mice model. Mech. Ageing Dev. 132: 573–582. DOI: 10.1016/j.mad.2011.10.005.
131. Lin XJ, Mei GP, Liu J, Li YL, Zuo D, Liu SJ, Zhao TB, Lin MT (2011) Therapeutic effects of melatonin on heatstroke-induced multiple organ dysfunction syndrome in rats. J. Pineal Res. 50: 436–444. DOI: 10.1111/j.1600-079X.2011.00863.x.
132. Tocharus J, Khonthun C, Chongthammakun S, Govitrapong P (2010) Melatonin attenuates methamphetamine-induced overexpression of pro-inflammatory cytokines in microglial cell lines. J. Pineal Res. 48: 347–352. DOI: 10.1111/j.1600-079X.2010.00761.x.
133. Mishra A, Paul S, Swarnakar S (2011) Downregulation of matrix metalloproteinase-9 by melatonin during prevention of alcohol-induced liver injury in mice. Biochimie 93: 854–866. DOI: 10.1016/j.biochi.2011.02.007.
134. Kim GD, Lee SE, Kim TH, Jin YH, Park YS, Park CS (2012) Melatonin suppresses acrolein-induced IL-8 production in human pulmonary fibroblasts. J. Pineal Res. 52: 356–364. DOI: 10.1111/j.1600-079X.2011.00950.x.
135. Yu L, Sun Y, Cheng L, Jin Z, Yang Y, Zhai M, Pei H, Wang X, Zhang H, Meng Q, Zhang Y (2014) Melatonin receptor‐mediated protection against myocardial ischemia/reperfusion injury: role of SIRT 1. J. Pineal Res. 57: 228-238. DOI: 10.1111/jpi.12161.
136. Brunet A, Sweeney LB, Sturgill JF, Chua KF, Greer PL, Lin Y, Tran H, Ross SE, Mostoslavsky R, Cohen HY, Hu LS (2004) Stress-dependent regulation of FOXO transcription factors by the SIRT1 deacetylase. Science 303: 2011-2015. DOI: 10.1126/science.1094637.
137. Alcendor RR, Gao S, Zhai P, Zablocki D, Holle E, Yu X, Tian B, Wagner T, Vatner SF, Sadoshima J (2007) Sirt1 regulates aging and resistance to oxidative stress in the heart. Circ. Res. 100: 1512-1521. DOI: 10.1161/01.RES.0000267723.65696.4a.
138. Yu L, Liang H, Dong X, Zhao G, Jin Z, Zhai M, Yang Y, Chen W, Liu J, Yi W, Yang J (2015) Reduced silent information regulator 1 signaling exacerbates myocardial ischemia–reperfusion injury in type 2 diabetic rats and the protective effect of melatonin. J. Pineal Res. 59: 376-390. DOI: 10.1111/jpi.12269.
139. Yu L, Li F, Zhao G, Yang Y, Jin Z, Zhai M, Yu W, Zhao L, Chen W, Duan W, Yu S (2015) Protective effect of berberine against myocardial ischemia reperfusion injury: role of Notch1/Hes1-PTEN/Akt signaling. Apoptosis 20: 796-810. DOI: 10.1007/s10495-015-1122-4.
140. Miele L (2006) Notch signaling. Clin. Cancer Res. 12: 1074-1079. DOI: 10.1158/1078-0432.ccr-05-2570.
141. Salmena L, Carracedo A, Pandolfi PP (2008) Tenets of PTEN tumor suppression. Cell 133: 403-414. DOI: 10.1016/j.cell.2008.04.013.
142. Yu L, Liang H, Lu Z, Zhao G, Zhai M, Yang Y, Yang J, Yi D, Chen W, Wang X, Duan W (2015) Membrane receptor‐dependent Notch1/Hes1 activation by melatonin protects against myocardial ischemia–reperfusion injury: in vivo and in vitro studies. J. Pineal Res. 59: 420-433. DOI: 10.1111/jpi.12272.
143. Luo B, Lin Y, Jiang S, Huang L, Yao H, Zhuang Q, Zhao R, Liu H, He C, Lin Z (2016) Endoplasmic reticulum stress eIF2 α–ATF4 pathway-mediated cyclooxygenase-2 induction regulates cadmium-induced autophagy in kidney. Cell death Dis. 7: e2251. DOI: 10.1038/cddis.2016.78.
144. Yu L, Li B, Zhang M, Jin Z, Duan W, Zhao G, Yang Y, Liu Z, Chen W, Wang S, Yang J (2016) Melatonin reduces PERK-eIF2α-ATF4-mediated endoplasmic reticulum stress during myocardial ischemia–reperfusion injury: role of RISK and SAFE pathways interaction. Apoptosis 21: 809-824. DOI: 10.1007/s10495-016-1246-1.
145. Yeung HM, Hung MW, Lau CF, Fung ML (2015) Cardioprotective effects of melatonin against myocardial injuries induced by chronic intermittent hypoxia in rats. J. Pineal Res. 58: 12-25. DOI: 10.1111/jpi.12190.
146. Prado NJ, Muñoz EM, Farias Altamirano LE, Aguiar F, Ponce Zumino AZ, Sánchez FJ, Miatello RM, Pueyo E, Diez ER (2020) Reperfusion arrhythmias increase after superior cervical ganglionectomy due to conduction disorders and changes in repolarization. Int. J. Mol. Sci .21: 1804. DOI: 10.3390/ijms21051804.
147. Xia CM, Shao CH, Xin L, Wang YR, Ding CN, Wang J, Shen LL, Li L, Cao YX, Zhu DN (2008) Effects of melatonin on blood pressure in stress‐induced hypertension in rats. Clin. Exp. Pharmacol. Physiol. 35: 1258-1264. DOI: 10.1111/j.1440-1681.2008.05000.x.
148. Prado NJ, Ferder L, Manucha W, Diez ER (2018) Anti-inflammatory effects of melatonin in obesity and hypertension. Curr. Hypertens. Rep. 20: 45. DOI: 10.1007/s11906-018-0842-6.
149. Szewczyk‐Golec K, Woźniak A, Reiter RJ (2015) Inter‐relationships of the chronobiotic, melatonin, with leptin and adiponectin: implications for obesity. J. Pineal Res. 59: 277-291. DOI: 10.1111/jpi.12257.
150. de Oliveira AC, Andreotti S, Farias Tda S, Torres-Leal FL, de Proença AR, Campaña AB, de Souza AH, Sertié RA, Carpinelli AR, Cipolla-Neto J, Lima FB (2012) Metabolic disorders and adipose tissue insulin responsiveness in neonatally STZ-induced diabetic rats are improved by longterm melatonin treatment. Endocrinology 153: 2178–2188. DOI: 10.1210/en.2011-1675.
151. Reiter RJ, Tan DX, Paredes SD, Fuentes-Broto L (2010) Beneficial effects of melatonin in cardiovascular disease. Ann. Med. 42: 276-285. DOI: 10.3109/07853890903485748.
152. Hu ZP, Fang XL, Fang N, Wang XB, Qian HY, Cao Z, Cheng Y, Wang BN, Wang Y (2013) Melatonin ameliorates vascular endothelial dysfunction, inflammation, and atherosclerosis by suppressing the TLR 4/NF‐κB system in high‐fat‐fed rabbits. J. Pineal Res. 55: 388-398. DOI: 10.1111/jpi.12085.
153. Ma S, Chen J, Feng J, Zhang R, Fan M, Han D, Li X, Li C, Ren J, Wang Y, Cao F (2018) Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and NLRP3 inflammasome inhibition. Oxid. Med. Cell. Longev. 2018: 9286458. DOI: 10.1155/2018/9286458.
154. Rudra DS, Pal U, Maiti NC, Reiter RJ, Swarnakar S (2013) Melatonin inhibits matrix metalloproteinase‐9 activity by binding to its active site. J. Pineal Res .54: 398-405. DOI: 10.1111/jpi.12034.
155. Fu Z, Jiao Y, Wang J, Zhang Y, Shen M, Reiter RJ, Xi Q and Chen Y (2020) Cardioprotective role of melatonin in acute myocardial infarction. Front. Physiol. 11: 366. DOI: 10.3389/fphys.2020.00366.
156. Nduhirabandi F, Lamont K, Albertyn Z, Opie LH, Lecour S (2016) Role of toll‐like receptor 4 in melatonin‐induced cardioprotection. J. Pineal Res. 60: 39-47. DOI: 10.1111/jpi.12286.
157. Sun H, Gusdon AM, Qu S (2016) Effects of melatonin on cardiovascular diseases: progress in the past year. Curr. Opin. Lipidol. 27: 408-413. DOI: 10.1097/MOL.0000000000000314.
158. Dominguez-Rodriguez A, Abreu-Gonzalez P, Jose M, Consuegra-Sanchez L, Piccolo R, Gonzalez-Gonzalez J, Garcia-Camarero T, del Mar Garcia-Saiz M, Aldea-Perona A, Reiter RJ, Caballero-Estevez N (2017) Usefulness of early treatment with melatonin to reduce infarct size in patients with ST-segment elevation myocardial infarction receiving percutaneous coronary intervention (from the melatonin adjunct in the acute myocardial infarction treated with angioplasty trial). Am. J. Cardiol. 120: 522-526. DOI:10.1016/j.amjcard.2017.05.018.
159. Dominguez-Rodriguez A, Abreu-Gonzalez P, Chen Y (2019) Cardioprotection and effects of melatonin administration on cardiac ischemia reperfusion: Insight from clinical studies. Melatonin Res. 2: 100-105. DOI: https://doi.org/https://doi.org/10.32794/mr11250024.
160. Han D, Wang Y, Chen J, Zhang J, Yu P, Zhang R, Li S, Tao B, Wang Y, Qiu Y, Xu M (2019) Activation of melatonin receptor 2 but not melatonin receptor 1 mediates melatonin‐conferred cardioprotection against myocardial ischemia/reperfusion injury. J. Pineal Res .67: e12571. DOI: 10.1111/jpi.12571.
161. Yang JB, Kang YM, Zhang C, Yu XJ, Chen WS (2019) Infusion of melatonin into the paraventricular nucleus ameliorates myocardial ischemia–reperfusion injury by regulating oxidative stress and inflammatory cytokines. J. Cardiovasc. Pharmacol. 74: 336-347. DOI: 10.1097/FJC.0000000000000711.
162. Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol.14: 88-98. DOI: 10.1038/nrendo.2017.151
163. Lu L, Ma J, Sun M, Wang X, Gao E, Lu L, Ren J, Yang L, Yang J (2020) Melatonin ameliorates MI-Induced cardiac remodeling and apoptosis through a JNK/p53-dependent mechanism in diabetes mellitus. Oxid. Med. Cell. Longev. 2020: 1535201. DOI: 10.1155/2020/1535201.
164. Zhou H, Yue Y, Wang J, Ma Q, Chen Y (2018) Melatonin therapy for diabetic cardiomyopathy: a mechanism involving Syk-mitochondrial complex I-SERCA pathway. Cell. Signal 47: 88-100. DOI: 10.1016/j.cellsig.2018.03.012.
165. Kandemir YB, Tosun V, Güntekin Ü (2019) Melatonin protects against streptozotocin-induced diabetic cardiomyopathy through the mammalian target of rapamycin (mTOR) signaling pathway. Adv. Clin. Exp. Med. 28: 1171-1177. DOI: 10.17219/acem/103799.
166. Che H, Wang Y, Li H, Li Y, Sahil A, Lv J, Liu Y, Yang Z, Dong R, Xue H, Wang L (2020) Melatonin alleviates cardiac fibrosis via inhibiting lncRNA MALAT1/miR‐141‐mediated NLRP3 inflammasome and TGF‐β1/Smads signaling in diabetic cardiomyopathy. FASEB J. 34: 5282-5298. DOI: 10.1096/fj.201902692R.
167. MacDonald IJ, Huang CC, Liu SC, Tang CH (2020) Reconsidering the role of melatonin in rheumatoid arthritis. Int. J. Mol. Sci. 21: 2877. DOI: 10.3390/ijms21082877.
168. Huang CC, Chiou CH, Liu SC, Hu SL, Su CM, Tsai CH, Tang CH (2019) Melatonin attenuates TNF‐α and IL‐1β expression in synovial fibroblasts and diminishes cartilage degradation: Implications for the treatment of rheumatoid arthritis. J. Pineal Res. 66: e12560. DOI: 10.1111/jpi.12560.
169. Conti A, Maestroni GJ (1996) Role of the pineal gland and melatonin in the development of autoimmune diabetes in non-obese diabetic mice. J. Pineal Res. 20: 164-172. DOI: 10.1111/j.1600-079x.1996.tb00253.x.
170. Lin GJ, Huang SH, Chen SJ, Wang CH, Chang DM, Sytwu HK (2013) Modulation by melatonin of the pathogenesis of inflammatory autoimmune diseases. Int. J. Mol. Sci. 14: 11742-11766. DOI: 10.3390/ijms140611742.
171. Mazzon E, Esposito E, Crisafulli C, Riccardi L, Muià C, Di Bella P, Meli R, Cuzzocrea S (2006) Melatonin modulates signal transduction pathways and apoptosis in experimental colitis. J. Pineal Res. 41: 363–373. DOI: 10.1111/j.1600-079X.2006.00378.x.
172. Chojnacki C, Wisniewska-Jarosinska M, Walecka-Kapica E, Klupinska G, Jaworek J, Chojnacki J (2011) Evaluation of melatonin effectiveness in the adjuvant treatment of ulcerative colitis. J. Physiol. Pharmacol .62: 327–334.
173. Hulten E, Mitchell J, Scally J, Gibbs B, Villines TC (2009) HIV positivity, protease inhibitor exposure and subclinical atherosclerosis: a systematic review and meta-analysis of observational studies. Heart 95: 1826-1835. DOI: 10.1136/hrt.2009.177774.
174. Luetkens JA, Doerner J, Schwarze-Zander C, Wasmuth JC, Boesecke C, Sprinkart AM, Schmeel FC, Homsi R, Gieseke J, Schild HH, Rockstroh JK (2016) Cardiac magnetic resonance reveals signs of subclinical myocardial inflammation in asymptomatic HIV-infected patients. Circ. Cardiovasc. Imaging. 9: e004091. DOI: 10.1161/CIRCIMAGING.115.004091.
175. Narciso P, Tozzi V, D’Offizi G, de Carli G, Orchi N, Galati V, Vincenzi L, Bellagamba R, Carvelli C, Puro V (2001) Metabolic and morphologic disorders in patients treated with hightly active antiretroviral therapy since primary HIV infection. Ann. NY Acad. Sci. 946: 214-222. DOI: 10.1111/j.1749-6632.2001.tb03914.x.
176. Nerone FR, Messias GF, Spack Jr M, Pupulin AR (2019) Effects of melatonin on wetabolic abnormalities in HIV patients treated with antiretroviral drugs. J. Adv. Med. Pharm. Sci. 16: 1-10. DOI: 10.9734/jamps/2019/v21i130121.
177. Talib WH (2018) Melatonin and cancer hallmarks. Molecules 23: 518. DOI: 10.3390/molecules23030518.
178. Li Y, Li S, Zhou Y, Meng X, Zhang JJ, Xu DP, Li HB (2017) Melatonin for the prevention and treatment of cancer. Oncotarget 8: 39896-39921. DOI: 10.18632/oncotarget.16379.
179. Liu R, Fu A, Hoffman AE, Zheng T, Zhu Y (2013) Melatonin enhances DNA repair capacity possibly by affecting genes involved in DNA damage responsive pathways. BMC Cell Biol. 14: 1. DOI: 10.1186/1471-2121-14-1.
180. Fischer TW, Kleszczyński K, Hardkop LH, Kruse N, Zillikens D (2013) Melatonin enhances antioxidative enzyme gene expression (CAT, GPx, SOD), prevents their UVR-induced depletion, and protects against the formation of DNA damage (8-hydroxy-20-deoxyguanosine) in ex vivo human skin. J. Pineal Res. 54: 303–312. DOI: 10.1111/jpi.12018.
181. Ghobadi A, Shirazi A, Najafi M, Kahkesh MH, Rezapoor S (2017) Melatonin ameliorates radiation-induced oxidative stress at targeted and nontargeted lung tissue. J. Med. Phys. 42: 241–244. DOI: 10.4103/jmp.JMP_60_17
182. Sliwinski T, Rozej W, Morawiec-Bajda A, Morawiec Z, Reiter R, Blasiak J (2007) Protective action of melatonin against oxidative DNA damage— Chemical inactivation versus base-excision repair. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 634: 220–227. DOI: 10.1016/j.mrgentox.2007.07.013.
183. Aydemir S, Akgün SG, Beceren A, Yüksel M, Kumaş M, Erdoğan N, Sardaş S, Omurtağ GZ. (2017) Melatonin ameliorates oxidative DNA damage and protects against formaldehyde-induced oxidative stress in rats. Int. J. Clin. Exp. Med. 10: 6250–6261.
184. Wu HJ, Liu C, Duan WX, Xu SC, He MD, Chen CH, Wang Y, Zhou Z, Yu ZP, Zhang L, Chen Y (2013) Melatonin ameliorates bisphenol A-induced DNA damage in the germ cells of adult male rats. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 752: 57–67. DOI: 10.1016/j.mrgentox.2013.01.005.
185. Erenberk U, Dundaroz R, Gok O, Uysal O, Agus S, Yuksel A, Yilmaz B, Kilic U (2014) Melatonin attenuates phenytoin sodium-induced DNA damage. Drug Chem. Toxicol. 37: 233–239. DOI: 10.3109/01480545.2013.838777.
186. Reiter RJ, Sharma R, Ma Q, Rosales-Corral S, Acuna-Castroviejo D, Escames G (2019) Inhibition of mitochondrial pyruvate dehydrogenase kinase: a proposed mechanism by which melatonin causes cancer cells to overcome cytosolic glycolysis, reduce tumor biomass and reverse insensitivity to chemotherapy. Melatonin Res. 2: 105-119. DOI: https://doi.org/10.32794/mr11250033.
187. Huang SH, Cao XJ, Wei W (2008) Melatonin decreases TLR3-mediated inflammatory factor expression via inhibition of NF-κB activation in respiratory syncytial virus-infected RAW264, 7 macrophages. J. Pineal Res. 45: 93–100. DOI: 10.1111/j.1600-079X.2008.00560.x.
188. Cho SY, Lee HJ, Jeong SJ, Lee HJ, Kim HS, Chen CY, Lee EO, Kim SH (2011) Sphingosine kinase 1 pathway is involved in melatonin-induced HIF-1α inactivation in hypoxic PC-3 prostate cancer cells. J. Pineal Res. 51: 87–93. DOI: 10.1111/j.1600-079X.2011.00865.x.
189. Pizarro JG, Yeste-Velasco M, Esparza JL, Verdaguer E, Pallàs M, Camins A, Folch J (2008) The antiproliferative activity of melatonin in B65 rat dopaminergic neuroblastoma cells is related to the downregulation of cell cycle-related genes. J. Pineal Res. 45: 8–16. DOI: 10.1111/j.1600-079X.2007.00548.x.
190. Hill SM, Frasch T, Xiang S, Yuan L, Duplessis T, Mao L (2009) Molecular mechanisms of melatonin anticancer effects. Integr. Cancer Ther. 8: 337–346. DOI: 10.1177/1534735409353332.
191. Mortezaee K, Najafi M, Farhood B, Ahmadi A, Potes Y, Shabeeb D, Musa AE (2019) Modulation of apoptosis by melatonin for improving cancer treatment efficiency: An updated review. Life Sci. 228: 228-241. DOI: 10.1016/j.lfs.2019.05.009.
192. Ferreira GM, Martinez M, Camargo IC, Domeniconi RF, Martinez FE, Chuffa LG (2014) Melatonin attenuates Her-2, p38 MAPK, p-AKT, and mTOR levels in ovarian carcinoma of ethanol-preferring rats. J. Cancer. 5: 728-735. DOI: 10.7150/jca.10196.
193. Sahna E, Parlakpinar H, Ozer MK, Ozturk F, Ozugurlu F, Acet A (2003) Melatonin protects against myocardial doxorubicin toxicity in rats: role of physiological concentrations. J. Pineal Res .35: 257-261. DOI: 10.1034/j.1600-079x.2003.00084.x.
194. Bilginoğlu A, Aydın D, Özsoy Ş, Aygün H (2014) Protective effect of melatonin on adriamycin-induced cardiotoxicity in rats. Turk. Kardiyol. Dern. Ars. 42: 265-273. DOI: 10.5543/tkda.2014.36089.
195. Guven A, Yavuz O, Cam M, Ercan F, Bukan N, Comunoglu C (2007) Melatonin protects against epirubicin-induced cardiotoxicity. Acta Histochem. 109: 52-60. DOI: 10.1016/j.acthis.2006.09.007.
196. Ghani EA, Kerr I, Dada R (2014) Grade 3 trastuzumab-induced neutropenia in breast cancer patient. J. Oncol. Pharm. Pract. 20: 154-157. DOI: 10.1177/1078155213487394.
197. Ozturk M, Ozler M, Kurt YG, Ozturk B, Uysal B, Ersoz N, Yasar M, Demirbas S, Kurt B, Acikel C, Oztas Y (2011) Efficacy of melatonin, mercaptoethylguanidine and 1400W in doxorubicin‐and trastuzumab‐induced cardiotoxicity. J. Pineal Res. 50: 89-96. DOI: 10.1111/j.1600-079X.2010.00818.x.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.