Protective effect of melatonin in atherosclerotic cardiovascular disease: A comprehensive review
Melatonin protects cardiovascular tissue from atherosclerosis
Abstract
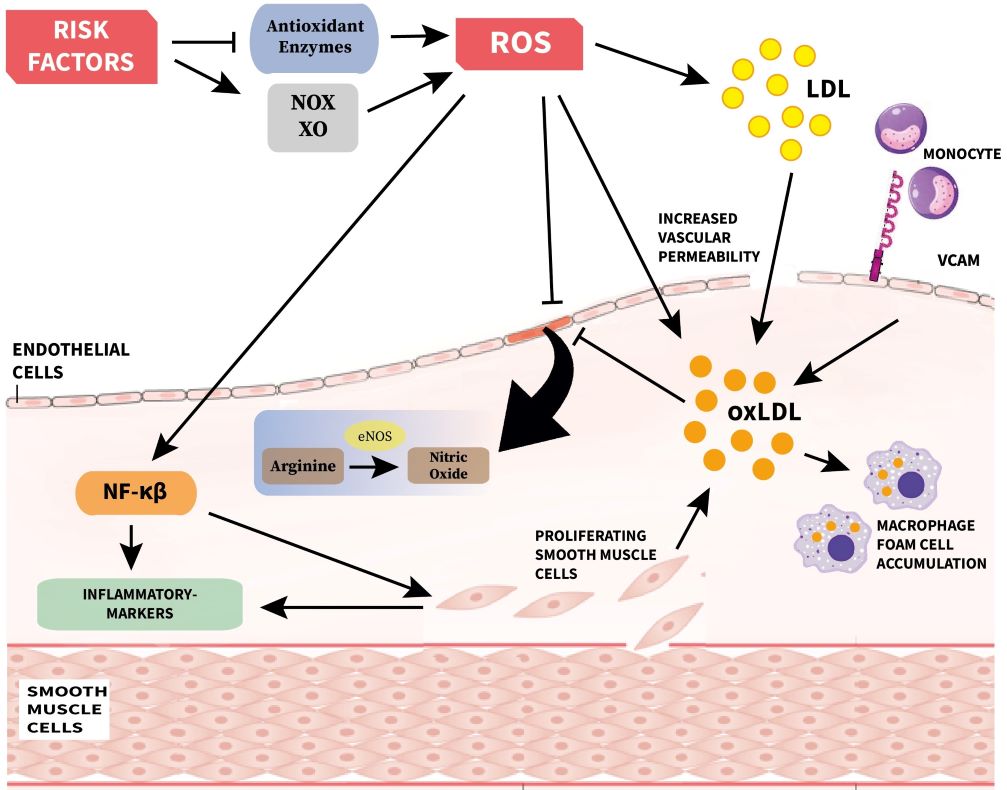
Heart failure is characterized by the heart losing its capacity to pump sufficient blood to match the body’s demand. It is caused by a variety of cardiovascular impairments. Among them, atherosclerosis is the most common one. Although, a variety of medicines selectively target this pathology, the death rate due to atherosclerosis associated heart disorders remain high. To address this issue, the use of antioxidants combined with conventional therapy to achieve synergistic effects has gained popularity. Melatonin is one of such antioxidants. In addition to its potent antioxidant activity, this molecule acts in harmony to protect the cardiovascular tissue. This review explores the various mechanisms by which melatonin protects the cardiovascular tissue. This information will contribute further insights into the role of melatonin in maintaining cardiovascular homeostasis in normal as well as in pathological conditions. It will also help us to better understand the potential synergistic effects of melatonin with conventional therapy to successfully target the heart failure associated with atherosclerosis.
References
2. Keys A, Taylor HL, Blackburn H, Brozek J, Anderson JT, Simonson E (1963) Coronary heart disease among Minnesota business and professional men followed fifteen years. Circulation. 28 (3): 381–395. DOI: 10.1161/01.CIR.28.3.381.
3. Ardies CM, Roberts CK (2014) Atherosclerosis. Diet Exerc. Chronic Dis. Biol. Basis Prev. 133–210. DOI: 10.1201/b16783.
4. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M et al. (2016) Executive summary: Heart disease and stroke statistics--2016 update: a report from the american heart association. Circulation 133 (4): 447–454. DOI: 10.1161/CIR.0000000000000366.
5. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP et al. (2019) Heart disease and stroke statistics-2019 update: A report from the american heart association. Circulation 139 (10): e56–e528. DOI: 10.1161/CIR.0000000000000659.
6. Maximilian Buja LM, McAllister HA (2015) Coronary artery disease: Pathological anatomy and pathogenesis. Cardiovasc. Med. 593–610. DOI: 10.1007/978-1-4471-2828-1_1.
7. Candore G, Vasto S, Colonna-Romano G, Lio D, Caruso M, Rea IM, Caruso C (2006) Atherosclerosis: The road ahead. Cell 104: 503-516. DOI: 10.1016/s0092-8674(01)00238-0.
8. Förstermann U (2008) Oxidative stress in vascular disease: causes, defense mechanisms and potential therapies. Nat. Clin. Pract. Cardiovasc. Med. 5 (6): 338–349. DOI: 10.1038/ncpcardio1211.
9. Bentzon JF, Otsuka F, Virmani R, Falk E (2014) Mechanisms of plaque formation and rupture. Circ. Res. 114 (12): 1852–1866. DOI: 10.1161/CIRCRESAHA.114.302721.
10. Tarocco A, Caroccia N, Morciano G, Wieckowski MR, Ancora G, Garani G, Pinton P (2019) Melatonin as a master regulator of cell death and inflammation: molecular mechanisms and clinical implications for newborn care. Cell Death Dis. 10 (4): 317. DOI: 10.1038/s41419-019-1556-7.
11. Chuang JI, Chen SS, Lin MT (1993) Melatonin decreases brain serotonin release, arterial pressure and heart rate in rats. Pharmacology 47 (2): 91–97. DOI: 10.1159/000139083.
12. Mullerwieland D, Behnke B, Koopmann K, Krone W (1994) Melatonin inhibits LDL receptor activity and cholesterol-synthesis in freshly isolated human mononuclear leukocytes. Biochem. Biophys. Res. Commun. 203 (1): 416–421. DOI: 10.1006/bbrc.1994.2198.
13. Reiter RJ, Tan DX (2003) Melatonin: A novel protective agent against oxidative injury of the ischemic/reperfused heart. Cardiovasc. Res. 58 (1): 10–19. DOI: 10.1016/S0008-6363(02)00827-1.
14. Reiter RJ, Tan D-X, Mayo JC, Sainz RM, Leon J, Czarnocki Z (2003) Melatonin as an antioxidant: biochemical mechanisms and pathophysiological implications in humans. Acta Biochim. Pol. 50 (4): 1129–1146. PMID: 14740000.
15. Lochner A, Genade S, Davids A, Ytrehus K, Moolman JA (2006) Short- and long-term effects of melatonin on myocardial post-ischemic recovery. J. Pineal Res. 40 (1): 56–63. DOI: 10.1111/j.1600-079X.2005.00280.x.
16. Andersen LPH, Gögenur I, Rosenberg J, Reiter RJ (2016) The safety of melatonin in humans. Clin. Drug Investig. 36 (3): 169–175. DOI: 10.1007/s40261-015-0368-5.
17. Reiter RJ, Mayo JC, Tan D-X, Sainz RM, Alatorre-Jimenez M, Qin L (2016) Melatonin as an antioxidant: under promises but over delivers. J. Pineal Res. 61 (3): 253–278. DOI: 10.1111/jpi.12360.
18. Falk E (2006) Pathogenesis of atherosclerosis. J. Am. Coll. Cardiol. 47 (8): C7–C12. DOI: 10.1016/j.jacc.2005.09.068.
19. Duarte MMMF, Rocha JBT, Moresco RN, Duarte T, Da Cruz IBM, Loro VL, Schetinger MRC (2009) Association between ischemia-modified albumin, lipids and inflammation biomarkers in patients with hypercholesterolemia. Clin. Biochem. 42 (7–8): 666–671. DOI: 10.1016/j.clinbiochem.2009.01.010.
20. Csonka C, Sárközy M, Pipicz M, Dux L, Csont T (2016) Modulation of hypercholesterolemia-induced oxidative/nitrative stress in the heart. Oxid. Med. Cell. Longev. 2016: 1-20. DOI: 10.1155/2016/3863726.
21. Viazzi F, Leoncini G, Ratto E, Parodi A, Falqui V, Conti N, Tomolillo C, Ravera G, Deferrari G, Pontremoli R (2008) Vascular permeability, blood pressure, and organ damage in primary hypertension. Hypertens Res. 31 (5): 873–879. DOI: 10.1291/hypres.31.873.
22. Mundi S, Massaro M, Scoditti E, Carluccio MA, Van Hinsbergh VWM, Iruela-Arispe ML, De Caterina R (2018) Endothelial permeability, LDL deposition, and cardiovascular risk factors-A review. Cardiovasc. Res. 114 (1): 35–52. DOI: 10.1093/cvr/cvx226.
23. Lassègue B, Griendling KK (2004) Reactive oxygen species in hypertension: An update. Am. J. Hypertens. 17 (9): 852–860. DOI: 10.1016/j.amjhyper.2004.02.004. DOI: 10.1016/j.amjhyper.2004.02.004.
24. Zimmermann R, Panzenböck U, Wintersperger A, Levak-Frank S, Graier W, Glatter O, Fritz G, Kostner GM, Zechner R (2001) lipoprotein lipase mediates the uptake of glycated LDL in fibroblasts, endothelial cells, and macrophages. Diabetes 50 (7): 1643–1653. DOI: 10.2337/diabetes.50.7.1643.
25. Avogaro A, Albiero M, Menegazzo L, De Kreutzenberg S, Fadini GP (2011) Endothelial dysfunction in diabetes: The role of reparatory mechanisms. Diabetes Care 34 (Suppl. 2). DOI: 10.2337/dc11-s239.
26. Volpe CMO, Villar-Delfino PH, Dos Anjos PMF, Nogueira-Machado JA (2018) Cellular death, reactive oxygen species (ROS) and diabetic complications. Cell Death Dis. 9 (2). DOI: 10.1038/s41419-017-0135-z.
27. Kelly AS, Jacobs DR, Sinaiko AR, Moran A, Steffen LM, Steinberger J (2010) Relation of circulating oxidized LDL to obesity and insulin resistance in children. Pediatr. Diabetes 11 (8): 552–555. DOI: 10.1111/j.1399-5448.2009.00640.x.
28. Björntorp P, Bergman H, Varnauskas E (1969) Plasma free fatty acid turnover rate in obesity. Acta Med. Scand. 185 (1–6): 351–356. DOI: 10.1111/j.0954-6820.1969.tb07347.x.
29. Boden G (2008) Obesity and free fatty acids. Endocrinol. Metab. Clin. North Am. 37 (3): 635–646. DOI: 10.1016/j.ecl.2008.06.007.
30. Klop B, Elte JWF, Cabezas MC (2013) Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 5 (4): 1218–1240. DOI: 10.3390/nu5041218.
31. Njajou OT, Kanaya AM, Holvoet P, Connelly S, Strotmeyer ES, Harris TB, Cummings SR, Hsueh WC (2009) Association between oxidized LDL, obesity and type 2 diabetes in a population-based cohort, the health, aging and body composition study. Diabetes Metab. Res. Rev. 25 (8): 733–739. DOI: 10.1002/dmrr.1011.
32. McEvoy JW, Nasir K, Defilippis AP, Lima JAC, Bluemke DA, Hundley WG, Barr RG, Budoff MJ, Szklo M, Navas-Acien A, Polak JF, Blumenthal RS, Post WS, Blaha MJ (2015) Relationship of cigarette smoking with inflammation and subclinical vascular disease: The multi-ethnic study of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 35 (4): 1002–1010. DOI: 10.1161/ATVBAHA.114.304960.
33. Pamukcu B, Oflaz H, Onur I, Cimen A, Nisanci Y (2011) Effect of cigarette smoking on platelet aggregation. Clin. Appl. Thromb. 17 (6). DOI: 10.1177/1076029610394440.
34. Messner B, Bernhard D (2014) Smoking and cardiovascular disease: Mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler. Thromb. Vasc. Biol. 34 (3): 509–515. DOI: 10.1161/ATVBAHA.113.300156.
35. Craig WY, Palomaki GE, Haddow JE (1989) Cigarette smoking and serum lipid and lipoprotein concentrations: An analysis of published data. Br. Med. J. 298 (6676): 784–788. DOI: 10.1136/bmj.298.6676.784.
36. Kamceva G, Arsova-Sarafinovska Z, Ruskovska T, Zdravkovska M, Kamceva-Panova L, Stikova E (2016) Cigarette smoking and oxidative stress in patients with coronary artery disease. Maced. J. Med. Sci. 4 (4): 636–640. DOI: 10.3889/oamjms.2016.117.
37. Wang JC, Bennett M (2012) Aging and atherosclerosis: Mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ. Res. 111 (2): 245–259. DOI: 10.1161/CIRCRESAHA.111.261388.
38. Fairweather D (2014) Sex differences in inflammation during atherosclerosis. Clin. Med. Insights Cardiol. 8 (Suppl. 3): 49–59. DOI: 10.4137/CMC.S17068.
39. Pandey AK, Blaha MJ, Sharma K, Rivera J, Budoff MJ, Blankstein R, Al-Mallah M, Wong ND, Shaw L, Carr J, O’Leary D, Lima JAC, Szklo M, Blumenthal RS, Nasir K (2014) Family history of coronary heart disease and the incidence and progression of coronary artery calcification: Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis 232 (2): 369–376. DOI: 10.1016/j.atherosclerosis.2013.11.042.
40. Liu W, Zhang Y, Yu CM, Ji QW, Cai M, Zhao YX, Zhou YJ (2015) Current understanding of coronary artery calcification. J. Geriatr. Cardiol. 12 (6): 668–675. DOI: 10.11909/j.issn.1671-5411.2015.06.012.
41. Lutgens E, Van Suylen RJ, Faber BC, Gijbels MJ, Eurlings PM, Bijnens AP, Cleutjens KB, Heeneman S, Daemen MJAP (2003) Atherosclerotic plaque rupture: Local or systemic process? Arterioscler. Thromb. Vasc. Biol. 23 (12): 2123–2130. DOI: 10.1161/01.ATV.0000097783.01596.E2.
42. Levy A, Moreno P (2006) Intraplaque hemorrhage. Curr. Mol. Med. 6 (5): 479–488. DOI: 10.2174/156652406778018626.
43. Saric M, Kronzon I (2012) Aortic atherosclerosis and embolic events. Curr. Cardiol. Rep. 14 (3): 342–349. DOI: 10.1007/s11886-012-0261-2.
44. Beckman JA, Ganz J, Creager MA, Ganz P, Kinlay S (2001) Relationship of clinical presentation and calcification of culprit coronary artery stenoses. Arterioscler. Thromb. Vasc. Biol. 21 (10): 1618–1622. DOI: 10.1161/hq0901.095554.
45. Rocha-Singh KJ, Zeller T, Jaff MR (2014) Peripheral arterial calcification: Prevalence, mechanism, detection, and clinical implications. Catheter. Cardiovasc. Interv. 83 (6). DOI: 10.1002/ccd.25387.
46. Maniscalco BS, Taylor KA (2004) Calcification in coronary artery disease can be reversed by EDTA-tetracycline long-term chemotherapy. Pathophysiology 11 (2): 95–101. DOI: 10.1016/j.pathophys.2004.06.001.
47. Luis H Arroyo RTL (1999) Mechanisms of plaque rupture: mechanical and biologic interactions. Cardiovasc. Res. 41 (2): 369–375. doi: 10.1016/s0008-6363(98)00308-3.
48. Rothwell PM (2007) Atherothrombosis and ischaemic stroke. Br. Med. J. 334 (7590): 379–380. DOI: 10.1136/bmj.38964.489051.80.
49. Ntaios G, Hart RG (2017) Embolic stroke. Circulation 136 (25): 2403–2405. DOI: 0.1161/CIRCULATIONAHA.117.030509.
50. Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S (2016) Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ. Res. 118 (4): 535–546. DOI: 10.1161/CIRCRESAHA.115.307611.
51. Hansson G K (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl. J. Med. 352 (16): 1685–1695. DOI: 10.1056/NEJMra043430.
52. Cahill PA, Redmond EM (2016) Vascular endothelium - Gatekeeper of vessel health. Atherosclerosis 248 : 97–109. DOI: 10.1016/j.atherosclerosis.2016.03.007.
53. Davignon J, Ganz P (2004) Role of endothelial dysfunction in atherosclerosis. Circulation 109 (23_suppl_1): III-27-III–32. DOI: 10.1161/01.CIR.0000131515.03336.f8.
54. Lum H, Malik AB (1996) Mechanisms of increased endothelial permeability. Can. J. Physiol. Pharmacol. 74 (7): 787–800. DOI: 10.1139/y96-081.
55. Gimbrone MA, García-Cardeña G (2016) Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ. Res. 118 (4): 620–636. DOI: 10.1161/CIRCRESAHA.115.306301.
56. Becker BF, Chappell D, Bruegger D, Annecke T, Jacob M (2010) Therapeutic strategies targeting the endothelial glycocalyx: acute deficits, but great potential. Cardiovasc. Res. 87 (2): 300–310. DOI: 10.1093/cvr/cvq137.
57. van den Berg BM, Spaan JAE, Rolf TM, Vink H (2006) Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation. Am. J. Physiol. Circ. Physiol. 290 (2): H915–H920. DOI: 10.1152/ajpheart.00051.2005.
58. Skålén K, Gustafsson M, Rydberg EK, Hultén LM, Wiklund O, Innerarity TL, Borén J (2002) Subendothelial retention of atherogenic lipoproteins in early atherosclerosis. Nature 417 (6890): 750–754. DOI: 10.1038/nature00804.
59. Badimon L, Storey RF, Vilahur G (2011) Update on lipids, inflammation and atherothrombosis. Thromb. Haemost. 105 (S 06): S34–S42. DOI: 10.1160/THS10-11-0717.
60. Leitinger N (2003) Oxidized phospholipids as modulators of inflammation in atherosclerosis. Curr. Opin. Lipidol. 14 (5): 421-430. DOI: 10.1097/00041433-200310000-00002.
61. Nakashima Y, Raines EW, Plump AS, Breslow JL, Ross R (1998) Upregulation of VCAM-1 and ICAM-1 at atherosclerosis-prone sites on the endothelium in the apoe-deficient mouse. Arterioscler. Thromb. Vasc. Biol. 18 (5): 842–851. DOI: 10.1161/01.atv.18.5.842.
62. Cybulsky MI, Gimbrone MA (1991) Endothelial expression of a mononuclear leukocyte adhesion molecule during atherogenesis. Science 251 (4995): 788–791. DOI: 10.1126/science.1990440.
63. Libby P, Okamoto Y, Rocha VZ, Folco E (2010) Inflammation in atherosclerosis: Transition from theory to practice. Circ. J. 74 (2): 213–220. DOI: 10.1253/circj.cj-09-0706.
64. Howe KL, Fish JE (2019) Transforming endothelial cells in atherosclerosis. Nat. Metab. 1 (9): 856–857. DOI: 10.1038/s42255-019-0100-5.
65. Young Hee Choi and A-MY (2019) Endothelial cell dysfunction and the pathobiology of atherosclerosis. Physiol. Behav. 176 (3): 139–148. DOI: 10.1161/CIRCRESAHA.115.306301.
66. Ludmer PL, Selwyn AP, Shook TL, Wayne RR, Mudge GH, Alexander RW, Ganz P (1986) Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N. Engl. J. Med. 315 (17): 1046–1051. DOI: 10.1056/NEJM198610233151702.
67. Kanter JE, Johansson F, LeBoeuf RC, Bornfeldt KE (2007) Do glucose and lipids exert independent effects on atherosclerotic lesion initiation or progression to advanced plaques? Circ. Res. 100 (6): 769–781. DOI: 10.1161/01.RES.0000259589.
68. Wang JC, Bennett M (2012) Aging and atherosclerosis. Circ. Res. 111 (2): 245–259. DOI: 10.1161/CIRCRESAHA.111.261388.
69. Feng S, Bowden N, Fragiadaki M, Souilhol C, Hsiao S, Mahmoud M, Allen S, Pirri D, Ayllon BT, Akhtar S, Thompson AAR, Jo H, Weber C, Ridger V, Schober A, Evans PC (2017) Mechanical activation of hypoxia-inducible factor 1α drives endothelial dysfunction at atheroprone sites. Arterioscler. Thromb. Vasc. Biol. 37 (11): 2087–2101. DOI: 10.1161/ATVBAHA.117.309249.
70. Wu D, Huang R-T, Hamanaka RB, Krause M, Oh M-J, Kuo C-H, Nigdelioglu R, Meliton AY, Witt L, Dai G, Civelek M, Prabhakar NR, Fang Y, Mutlu GM (2017) HIF-1α is required for disturbed flow-induced metabolic reprogramming in human and porcine vascular endothelium. Elife 6 : e25217. DOI: 10.7554/eLife.25217.
71. Ross R, Glomset JA (1973) Atherosclerosis and the arterial smooth muscle cell. Science 180 (4093): 1332–1339. DOI: 10.1126/science.180.4093.1332.
72. Metz RP, Patterson JL, Wilson E (2012) Vascular smooth muscle cells: Isolation, culture, and characterization. Methods Mol. Biol. 843 : 169–176. DOI: 10.1007/978-1-61779-523-7_16.
73. Basatemur GL, Jorgensen HF, Clarke MCH, Bennett MR, Mallat Z (2019) Vascular smooth muscle cells in atherosclerosis. Nat. Rev. Cardiol. 16 (12): 727–744. DOI: 10.1038/s41569-019-0227-9.
74. Ye GJC, Nesmith AP, Parker KK (2014) The role of mechanotransduction on vascular smooth muscle myocytes cytoskeleton and contractile function. Anat. Rec. 297 (9): 1758–1769. DOI: 0.1002/ar.22983.
75. Osol G (1995) Mechanotransduction by vascular smooth muscle. J. Vasc. Res. 32 (5): 275–292. DOI: 10.1159/000159102.
76. Gunst SJ, Zhang W (2008) Actin cytoskeletal dynamics in smooth muscle: A new paradigm for the regulation of smooth muscle contraction. Am. J. Physiol. - Cell Physiol. 295 (3): C576-87. DOI: 10.1152/ajpcell.00253.2008.
77. Langton PD (1993) Calcium channel currents recorded from isolated myocytes of rat basilar artery are stretch sensitive. J. Physiol. 471 (1): 1–11. DOI: 10.1113/jphysiol.1993.sp019887.
78. Kolodgie FD, Burke AP, Nakazawa G, Virmani R (2007) Is pathologic intimal thickening the key to understanding early plaque progression in human atherosclerotic disease? Arterioscler. Thromb. Vasc. Biol. 27 (5): 986–989. DOI: 10.1161/ATVBAHA.0000258865.44774.41.
79. Li H, Cybulsky MI, Gimbrone Jr MA, Libby P (1993) Inducible expression of vascular cell adhesion molecule-1 by vascular smooth muscle cells in vitro and within rabbit atheroma. Am. J. Pathol. 143 (6): 1551–1559. PMID: 7504883.
80. Ross R (1999) Atherosclerosis — An inflammatory disease. N. Engl. J. Med. 340 (2): 115–126. DOI: 10.1056/NEJM199901143400207.
81. Campbell GR CJ (1990) The Phenotypes of smooth muscle expressed in human atheroma. Ann. N. Y. Acad. Sci. 598 (1): 143–158. DOI: 10.1111/j.1749-6632.1990.tb42286.x.
82. Thyberg J, Blomgren K, Hedin U, Dryjski M (1995) Phenotypic modulation of smooth muscle cells during the formation of neointimal thickenings in the rat carotid artery after balloon injury: an electron-microscopic and stereological study. Cell Tissue Res. 281 (3): 421–433. DOI: 10.1007/BF00417860.
83. Hao H, Gabbiani G, Bochaton-Piallat M-L (2003) Arterial smooth muscle cell heterogeneity. Arterioscler. Thromb. Vasc. Biol. 23 (9): 1510–1520. DOI: 10.1161/01.ATV.0000090130.85752.ED.
84. Walker LN, Bowen-Pope DF, Ross R, Reidy MA (1986) Production of platelet-derived growth factor-like molecules by cultured arterial smooth muscle cells accompanies proliferation after arterial injury. Proc. Natl. Acad. Sci. 83 (19): 7311–7315. DOI: 10.1073/pnas.83.19.7311.
85. Orlandi A, Ehrlich HP, Ropraz P, Spagnoli LG, Gabbiani G (1994) Rat aortic smooth muscle cells isolated from different layers and at different times after endothelial denudation show distinct biological features in vitro. Arterioscler. Thromb. A J. Vasc. Biol. 14 (6): 982–989. DOI: 10.1161/01.ATV.14.6.982.
86. Bochaton-Piallat M-L, Ropraz P, Gabbiani F, Gabbiani G (1996) Phenotypic heterogeneity of rat arterial smooth muscle cell clones: Implications for the development of experimental intimal thickening. Arterioscler. Thromb. Vasc. Biol. 16 (6): 815–820. DOI: 10.1161/01.atv.16.6.815.
87. Ip JH, Fuster V, Badimon L, Badimon J, Taubman MB, Chesebro JH (1990) Syndromes of accelerated atherosclerosis: Role of vascular injury and smooth muscle cell proliferation. J. Am. Coll. Cardiol. 15 (7): 1667–1687. DOI: 10.1016/0735-1097(90)92845-s.
88. Sano H, Ueda Y, Takakura N, Takemura G, Doi T, Kataoka H, Murayama T, Xu Y, Sudo T, Nishikawa S, Nishikawa S-I, Fujiwara H, Kita T, Yokode M (2002) Blockade of platelet-derived growth factor receptor-beta pathway induces apoptosis of vascular endothelial cells and disrupts glomerular capillary formation in neonatal mice. Am. J. Pathol. 161 (1): 135–143. DOI: 10.1016/s0002-9440(10)64165-x.
89. Andreeva ER, Pugach IM, Orekhov AN (1997) Subendothelial smooth muscle cells of human aorta express macrophage antigen in situ and in vitro. Atherosclerosis 135 (1): 19–27. DOI: 10.1016/s0021-9150(97)00136-6.
90. Rong JX, Shapiro M, Trogan E, Fisher EA (2003) Transdifferentiation of mouse aortic smooth muscle cells to a macrophage-like state after cholesterol loading. Proc. Natl. Acad. Sci. 100 (23): 13531–13536. DOI: 10.1073/pnas.1735526100.
91. Shankman LS, Gomez D, Cherepanova OA, Salmon M, Alencar GF, Haskins RM, Swiatlowska P, Newman AAC, Greene ES, Straub AC, Isakson B, Randolph GJ, Owens GK (2015) KLF4-dependent phenotypic modulation of smooth muscle cells has a key role in atherosclerotic plaque pathogenesis. Nat. Med. 21 (6): 628–637. DOI: 10.1038/nm.3866.
92. Orr AW, Hastings NE, Blackman BR, Wamhoff BR (2010) Complex regulation and function of the inflammatory smooth muscle cell phenotype in atherosclerosis. J. Vasc. Res. 47 (2): 168–180. DOI: 10.1159/000250095.
93. Allahverdian S, Chaabane C, Boukais K, Francis GA, Bochaton-Piallat M-L (2018) Smooth muscle cell fate and plasticity in atherosclerosis. Cardiovasc. Res. 114 (4): 540–550. DOI: 10.1093/cvr/cvy022.
94. Chistiakov DA, Orekhov AN, Bobryshev Y V (2015) Vascular smooth muscle cell in atherosclerosis. Acta Physiol. 214 (1): 33–50. DOI: 10.1038/s41569-019-0227-9.
95. Tabas I, García-Cardena G, Owens GK (2015) Recent insights into the cellular biology of atherosclerosis. J. Cell Biol. 209 (1): 13–22. DOI: 10.1083/jcb.201412052.
96. Allahverdian S, Pannu PS, Francis GA (2012) Contribution of monocyte-derived macrophages and smooth muscle cells to arterial foam cell formation. Cardiovasc. Res. 95 (2): 165–172. DOI: 10.1093/cvr/cvs094.
97. Costales P, Fuentes-Prior P, Castellano J, Revuelta-Lopez E, Corral-Rodríguez MÁ, Nasarre L, Badimon L, Llorente-Cortes V (2015) K domain CR9 of low density lipoprotein (LDL) receptor-related protein 1 (LRP1) is critical for aggregated LDL-induced foam cell formation from human vascular smooth muscle cells. J. Biol. Chem. 290 (24): 14852–14865. DOI: 10.1074/jbc.M115.638361.
98. Frontini MJ, O’Neil C, Sawyez C, Chan BMC, Huff MW, Pickering JG (2009) Lipid incorporation inhibits src-dependent assembly of fibronectin and type i collagen by vascular smooth muscle cells. Circ. Res. 104 (7): 832–841. DOI: 10.1161/CIRCRESAHA.108.187302.
99. Salabei JK, Hill BG (2013) Mitochondrial fission induced by platelet-derived growth factor regulates vascular smooth muscle cell bioenergetics and cell proliferation. Redox Biol. 1 (1): 542–551. DOI: 10.1016/j.redox.2013.10.011.
100. Chiong M, Cartes-Saavedra B, Norambuena-Soto I, Mondaca-Ruff D, Morales PE, García-Miguel M, Mellado R (2014) Mitochondrial metabolism and the control of vascular smooth muscle cell proliferation. Front. cell Dev. Biol. 2 : 72. DOI: 10.3389/fcell.2014.00072.
101. Gutteridge JMC (1995) Lipid peroxidation and antioxidants as biomarkers of tissue damage. Clin. Chem. 41 (12 (2)): 1819–1828. PMID: 7497639.
102. Victor V M, Apostolova N, Herance R, Hernandez-Mijares A, Rocha M (2009) Oxidative stress and mitochondrial dysfunction in atherosclerosis: mitochondria-targeted antioxidants as potential therapy. Curr. Med. Chem. 16 (35): 4654–4667. DOI: 10.2174/092986709789878265.
103. Schieber M, Chandel NS (2014) ROS function in redox signaling and oxidative stress. Curr. Biol. 24 (10): R453–R462. DOI: 10.1016/j.cub.2014.03.034.
104. Li H, Witte K, August M, Brausch I, Gödtel-Armbrust U, Habermeier A, Closs EI, Oelze M, Münzel T, Forstermann U (2006) Reversal of endothelial nitric oxide synthase uncoupling and up-regulation of endothelial nitric oxide synthase expression lowers blood pressure in hypertensive rats. J. Am. Coll. Cardiol. 47 (12): 2536–2544. DOI: 10.1016/j.jacc.2006.01.071.
105. Warnholtz A, Nickenig G, Schulz E, Macharzina R, Bräsen JH, Skatchkov M, Heitzer T, Stasch JP, Griendling KK, Harrison DG, Böhm M, Meinertz T, Münzel T (1999) Increased NADH-oxidase mediated superoxide production in the early stages of atherosclerosis. Circulation 99 (15): 2027–2033. DOI: 10.1161/01.cir.99.15.2027.
106. Hink U, Li H, Mollnau H, Oelze M, Matheis E, Hartmann M, Skatchkov M, Thaiss F, Stahl RAK, Warnholtz A, Meinertz T, Griendling K, Harrison DG, Forstermann U, Munzel T (2001) Mechanisms underlying endothelial dysfunction in diabetes mellitus. Circ. Res. 88 (2): 14–22. DOI: 10.1161/01.res.88.2.e14.
107. Mueller CFH, Laude K, McNally JS, Harrison DG (2005) ATVB in focus: redox mechanisms in blood vessels. Arterioscler. Thromb. Vasc. Biol. 25 (2): 274—278. DOI: 10.1161/01.ATV.0000149143.04821.eb.
108. Fukui T, Ishizaka N, Rajagopalan S, Laursen JB, Capers IV Q, Taylor WR, Harrison DG, De Leon H, Wilcox JN, Griendling KK (1997) p22phox mRNA expression and NADPH oxidase activity are increased in aortas from hypertensive rats. Circ. Res. 80 (1): 45–51. DOI: 10.1161/01.res.80.1.45.
109. Matsuno K, Yamada H, Iwata K, Jin D, Katsuyama M, Matsuki M, Takai S, Yamanishi K, Miyazaki M, Matsubara H, Yabe-Nishimura C (2005) Nox1 is involved in angiotensin II-mediated hypertension: A study in Nox1-deficient mice. Circulation 112 (17): 2677–2685. DOI: 10.1161/CIRCULATIONAHA.105.573709.
110. Griendling KK (2004) Novel NAD(P)H oxidases in the cardiovascular system. Heart 90 (5): 491–493. DOI: 10.1136/hrt.2003.029397.
111. Ohara Y, Peterson TE, Harrison DG (1993) Hypercholesterolemia increases endothelial superoxide anion production. J. Clin. Invest. 91 (6): 2546–2551. DOI: 10.1172/JCI116491.
112. Förstermann U, Münzel T (2006) Endothelial nitric oxide synthase in vascular disease: From marvel to menace. Circulation 113 (13): 1708–1714. DOI: 10.1161/CIRCULATIONAHA.105.602532.
113. Stocker R, Keaney JF (2005) New insights on oxidative stress in the artery wall. J. Thromb. Haemost. 3 (8): 1825–1834. DOI: 10.1111/j.1538-7836.2005.01370.x.
114. Viedt C, Soto U, Krieger-Brauer HI, Fei J, Elsing C, Kübler W, Kreuzer J (2000) Differential activation of mitogen-activated protein kinases in smooth muscle cells by angiotensin II: Involvement of p22phox and reactive oxygen species. Arterioscler. Thromb. Vasc. Biol. 20 (4): 940–948. DOI: 10.1161/01.ATV.20.4.940.
115. Kunsch C, Medford RM (1999) Oxidative stress as a regulator of gene expression in the vasculature. Circ. Res. 85 (8): 753–766. DOI: 10.1161/01.res.85.8.753.
116. Devary Y, Rosette C, Didonato JA, Karin M (1993) NF-κB activation by ultraviolet light not dependent on a nuclear signal. Science 261 (5127): 1442–1445. DOI: 10.1126/science.8367725.
117. Fruchart JC, Nierman MC, Stroes ESG, Kastelein JJP, Duriez P (2004) New risk factors for atherosclerosis and patient risk assessment. Circulation 109 (23 SUPPL.). DOI: 10.1161/01.CIR.0000131513.33892.5b.
118. Fowkes FGR, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, Norman PE, Sampson UKA, Williams LJ, Mensah GA, Criqui MH (2013) Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 382 (9901): 1329–1340. DOI: 10.1016/S0140-6736(13)61249-0.
119. Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N. Engl. J. Med. 338 (23): 1650–1656. DOI: 10.1056/NEJM199806043382302.
120. Orekhov AN, Sobenin IA, Revin V V., Bobryshev Y V. (2015) Development of antiatherosclerotic drugs on the basis of natural products using cell model approach. Oxid. Med. Cell. Longev. 2015 (2015): 1–11. DOI: 10.1155/2015/463797.
121. Letra-Vilela R, Sánchez-Sánchez AM, Rocha AM, Martin V, Branco-Santos J, Puente-Moncada N, Santa-Marta M, Outeiro TF, Antolín I, Rodriguez C, Herrera F (2016) Distinct roles of N-acetyl and 5-methoxy groups in the antiproliferative and neuroprotective effects of melatonin. Mol. Cell. Endocrinol. 434 : 238–249. DOI: 10.1016/j.mce.2016.07.012.
122. Majumder R, Datta M, Chattopadhyay A, Bandyopadhyay D (2021) Melatonin promotes gastric healing by modulating the components of matrix metalloproteinase signaling pathway: a novel scenario for gastric ulcer management. Melatonin Res. 4 (2): 213–231. DOI: 10.32794/mr11250092.
123. Reiter RJ, Tan DX, Gitto E, Sainz RM, Mayo JC, Leon J, Manchester LC, Vijayalaxmi A, Kilic E, Kilic Ü (2004) Pharmacological utility of melatonin in reducing oxidative cellular and molecular damage. Pol. J. Pharmacol. 56 (2): 159–170. PMID: 15156066.
124. Karbownik M, Reiter RJ (2000) Antioxidative effects of melatonin in protection against cellular damage caused by ionizing radiation. Proc. Soc. Exp. Biol. Med. 225 (1): 9–22. DOI: 10.1046/j.1525-1373.2000.22502.x.
125. Reiter RJ (1991) Melatonin: The chemical expression of darkness. Mol. Cell. Endocrinol. 79 (1–3): C153–C158. DOI: 10.1016/0303-7207(91)90087-9.
126. Reiter RJ (1998) Cytoprotective properties of melatonin: Presumed association with oxidative damage and aging. Nutrition 14 (9): 691–696. DOI: 10.1016/s0899-9007(98)00064-1.
127. Srinivasan V, Maestroni GJM, Cardinali DP, Esquifino AI, Pandi Perumal SR, Miller SC (2005) Melatonin, immune function and aging. Immun. Ageing 2: 17. DOI: 10.1186/1742-4933-2-17.
128. Tan DX, Manchester LC, Reiter RJ, Qi WB, Karbownik M, Calvoa JR (2000) Significance of melatonin in antioxidative defense system: Reactions and products. NeuroSignals 9 (3–4): 137–159. DOI: 10.1159/000014635.
129. Tengattini S, Reiter RJ, Tan DX, Terron MP, Rodella LF, Rezzani R (2008) Cardiovascular diseases: Protective effects of melatonin. J. Pineal Res. 44 (1): 16–25. DOI: 10.1111/j.1600-079X.2007.00518.x.
130. Cardinali DP (2019) Melatonin: Clinical perspectives in neurodegeneration. Front. Endocrinol. 10: 480. DOI: 10.3389/fendo.2019.00480.
131. Majumder R, Datta M, Pal PK, Bhattacharjee B, Chattopadhyay A, Bandyopadhyay D (2019) Protective mechanisms of melatonin on caprine spleen injury induced by cadmium (Cd): an in vitro study. Melatonin Res. 2 (3): 57–75. DOI: 10.32794/11250031.
132. Sandoo A, Veldhuijzen van Zanten JJC., Metsios GS, Carroll D, Kitas GD (2015) The endothelium and its role in regulating vascular tone. Open Cardiovasc. Med. J. 4 (1): 302–312. DOI: 10.2174/1874192401004010302.
133. Dominguez-Rodriguez A, Abreu-Gonzalez P, Sanchez-Sanchez JJ, Kaski JC, Reiter RJ (2010) Melatonin and circadian biology in human cardiovascular disease. J. Pineal Res. 49 (1): 14–22. DOI: 10.1111/j.1600-079X.2010.00773.x.
134. Naaz S, Mishra S, Pal PK, Chattopadhyay A, Das AR, Bandyopadhyay D (2020) Activation of SIRT1/PGC 1α/SIRT3 pathway by melatonin provides protection against mitochondrial dysfunction in isoproterenol induced myocardial injury. Heliyon 6 (10): e05159. DOI: 10.1016/j.heliyon.2020.e05159.
135. Zhou J, Zhang S, Zhao X, Wei T (2008) Melatonin impairs NADPH oxidase assembly and decreases superoxide anion production in microglia exposed to amyloid-β1-42. J. Pineal Res. 45 (2): 157–165. DOI: 10.1111/j.1600-079X.2008.00570.x.
136. Favero G, Rodella LF, Reiter RJ, Rezzani R (2014) Melatonin and its atheroprotective effects: A review. Mol. Cell. Endocrinol. 382 (2): 926–937. DOI: 10.1016/j.mce.2013.11.016.
137. Hu ZP, Fang XL, Fang N, Wang XB, Qian HY, Cao Z, Cheng Y, Wang BN, Wang Y (2013) Melatonin ameliorates vascular endothelial dysfunction, inflammation, and atherosclerosis by suppressing the TLR4/NF-κB system in high-fat-fed rabbits. J. Pineal Res. 55 (4): 388–398. DOI: 10.1111/jpi.12085.
138. Li HY, Leu YL, Wu YC, Wang SH (2019) Melatonin inhibits in vitro smooth muscle cell inflammation and proliferation and atherosclerosis in apolipoprotein e-deficient Mice. J. Agric. Food Chem. 67 (7): 1889–1901. DOI: 10.1021/acs.jafc.8b06217.
139. Lotufo CMC, Yamashita CE, Farsky SHP, Markus RP (2006) Melatonin effect on endothelial cells reduces vascular permeability increase induced by leukotriene B4. Eur. J. Pharmacol. 534 (1–3): 258–263. DOI: 10.1016/j.ejphar.2006.01.050.
140. Tang ST, Su H, Zhang Q, Tang HQ, Wang CJ, Zhou Q, Wei W, Zhu HQ, Wang Y (2016) Melatonin attenuates aortic endothelial permeability and arteriosclerosis in streptozotocin-induced diabetic rats: Possible role of MLCK- and MLCP-dependent MLC phosphorylation. J. Cardiovasc. Pharmacol. Ther. 21 (1): 82–92. DOI: 10.1177/1074248415583090.
141. Lee S, Byun J, Park M, Kim SW, Lee S, Kim J, Lee I, Choi Y, Park K (2020) Melatonin inhibits vascular smooth muscle cell proliferation and apoptosis through upregulation of Sestrin2. Exp. Ther. Med. 19 (6): 3454. DOI: 10.3892/etm.2020.8638.
142. Lee JH, Budanov A V., Karin M (2013) Sestrins orchestrate cellular metabolism to attenuate aging. Cell Metab. 18 (6): 792–801. DOI: 10.1016/j.cmet.2013.08.018.
143. Ro SH, Semple I, Ho A, Park HW, Lee JH (2015) Sestrin2, a regulator of thermogenesis and mitohormesis in brown adipose tissue. Front. Endocrinol. 6: 114. DOI: 10.3389/fendo.2015.00114.
144. Suofu Y, Li W, Jean-Alphonse FG, Jia J, Khattar NK, Li J et al. (2017) Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release. Proc. Natl. Acad. Sci. 114 (38): E7997–E8006. DOI: 10.1073/pnas.1705768114.

This work is licensed under a Creative Commons Attribution 4.0 International License.
For all articles published in Melatonin Res., copyright is retained by the authors. Articles are licensed under an open access Creative Commons CC BY 4.0 license, meaning that anyone may download and read the paper for free. In addition, the article may be reused and quoted provided that the original published version is cited. These conditions allow for maximum use and exposure of the work, while ensuring that the authors receive proper credit.
In exceptional circumstances articles may be licensed differently. If you have specific condition (such as one linked to funding) that does not allow this license, please mention this to the editorial office of the journal at submission. Exceptions will be granted at the discretion of the publisher.